In the previous part, we discussed the indications and contraindications for each retention type and examined detailed methods to mitigate the disadvantages and limitations of cement retention. This article will analyze the features of screw retention and address its potential challenges.
Screw Retention: Features and Recommendations for Use
We will begin by examining less ideal applications before moving to more reliable and durable approaches.
Let’s revisit the issue of errors in prosthesis framework fabrication and deviations during installation. Similar to construction, a small error at the foundation (e.g., 5-10 mm) can magnify significantly at higher levels, resulting in deviations of 30-40 cm for a 3-4 story building, or 1.4-1.7 meters for a 10-15 story building.
While prosthetic deviations aren’t typically this large, even a small angular error of 2-5° during fabrication can lead to noticeable gaps at the implant-abutment or abutment-prosthesis interface. These gaps not only create pathways for microflora penetration and biofilm formation but also allow for micromovement of the structure. This can lead to screw loosening (best-case scenario) or even component or implant fracture (worst-case scenario).
The following illustration and table (previously shown in Part 1) demonstrate this point. The picture clearly shows the difference between screw retention directly to an implant (left) and screw retention to a multi-unit abutment (MUA) (right). We see two designs with approximately the same angular deviation from the planned position. A significant difference is visible in the resulting deviation at the occlusal aspect of the structure, stemming from the difference in the lever arm height.
With direct-to-implant retention, the abutment component acts as a long lever arm, measured from the implant platform. This lever arm height is typically 9-15 mm. Furthermore, a long abutment component seated with a gap creates leverage that continuously stresses the implant neck and the retaining screw. This increases the risk of screw loosening or fracture, abutment damage, or even implant failure.
On the other hand, the same angular misfit when attaching the framework to an MUA results in a much smaller deviation at the top of the restoration because the lever arm is shorter (measured from the MUA platform). Moreover, the MUA itself should seat fully and passively onto the implant. Therefore, any risk of screw loosening or fracture primarily concerns the prosthetic screw connecting the frame to the MUA, not the abutment screw holding the MUA to the implant. The likelihood of damaging the MUA itself is minimal, and the risk of implant complications due to superstructure misfit is significantly reduced.
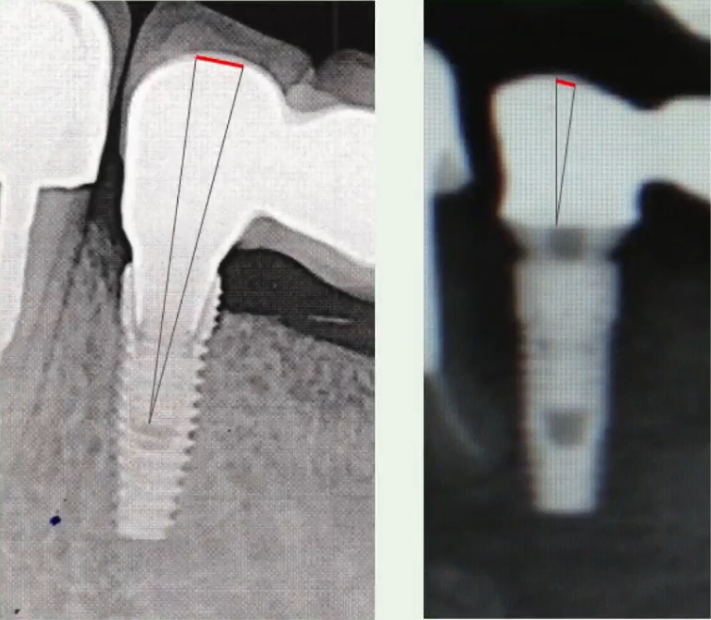
Comparison of framework deviation with screw retention directly to an implant versus to a multi-unit abutment (MUA): Using MUAs significantly lowers the likelihood of complications YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The table below illustrates that the longer the lever arm, the greater the final deviation from the planned position for a given angular misfit. These data confirm the advantages of using MUAs compared to direct screw retention onto implants. The average effective lever arm height for a direct screw-retained restoration (crown + abutment component) is often around 15 mm; with an angular misfit of 5°, we get a clinically significant deviation of 1.3 mm at the occlusal aspect. Whereas with a shorter lever arm height of 5 mm (typical above an MUA platform), the same 5° misfit results in a more acceptable deviation of only 0.43 mm. The restorative platform height of many standard MUAs is around 3.5-5.5 mm, but low-profile options like the XGate V-type MUA feature a height of only 1.5 mm, further reducing the lever arm effect. Therefore, a restoration with an effective lever arm of 5 mm above the MUA platform is common for screw retention on MUAs.
| Lever Arm Height (from screw edge to the top of the crown), mm | Angular Misfit 2° | Angular Misfit 5° |
| Resulting Linear Deviation, mm | Resulting Linear Deviation, mm | |
| 5 | 0.17 | 0.43 |
| 10 | 0.35 | 0.87 |
| 15 | 0.52 | 1.3 |
| 20 | 0.7 | 1.75 |
Compounding the issue, an angular misfit of 2° is virtually impossible to detect visually during restoration placement. Yet, the resulting gaps and micromovement can lead to significant complications.
Consider another example where the screw-retained crown fails to seat completely. Let’s analyze the reason.

The implant axis is not ideally centered relative to the planned crown contour, and the adjacent natural tooth (#45) is mesially tilted. On the distal side (contact with tooth #47), the contact aligns with the restoration’s path of insertion. However, on the mesial side (contact with tooth #45), the tilted adjacent tooth creates an interference. This mesial contact prevents the restoration from fully seating along its intended path of insertion. The illustration highlights this interference.
We could adjust (grind) the proximal contact on the crown, allowing it to seat, but this would create an open contact between the prosthesis and tooth #45, which is undesirable (leading to food impaction). Alternatively, the adjacent tooth could be orthodontically uprighted or restored to achieve parallel contacts, but this involves treating other teeth.
For single crowns, direct-to-implant screw retention is a common approach. While compromises may be necessary in such single-unit cases (like careful adjustment), for multiple-unit restorations (bridges), MUAs are strongly recommended to manage such issues more predictably. Failure to use MUAs in multi-unit situations with challenging paths of insertion or minor inaccuracies can lead to problems illustrated in the radiographs below. In both images, we can see gaps between the abutment components and the implant platforms, indicating a lack of passive fit.


There are two bridges with screw retention and in both cases there are visible problems with the fit; there are noticeable gaps in between the internal hex and the implant body YouTube / Dr. Kamil Khabiev / Dental Guru Academy
In these examples, the implants are installed relatively parallel, with an angular deviation between them of only 3-4°. Despite this slight deviation, the direct screw-retained abutments do not seat passively. The situation might be exacerbated by the internal hex connection type; a conical connection is often considered more forgiving of minor angular misfits compared to flat-to-flat hex connections.
Some clinicians might proceed with definitive placement despite a poor fit. The restoration might function for a period, but the eventual outcome is often component failure, as shown below.

Broken denture due to misfit of restoration YouTube / Dr. Kamil Khabiev / Dental Guru Academy
With such a misfit, the screws bear excessive occlusal load instead of it being distributed between the screws and a precisely fitting connection interface. Under dynamic and multidirectional masticatory forces, the screws are prone to loosening or fracture. Fortunately, in this instance, the screws failed first (acting like a mechanical fuse), preserving the implants. Note the plaque accumulation on the screws, a consequence of the large gaps at the implant-abutment interface.
Plaque and deposits also accumulate at the interface itself. Such contamination can lead to peri-implant mucositis or peri-implantitis. It’s worth noting that some bacterial ingress occurs even with well-fitting components due to the inherent microgap at any implant-abutment interface. Bacterial dimensions allow penetration into this space.

Deposits at the implant-abutment interface, difficult to access for cleaning without prosthesis removal YouTube / Dr. Kamil Khabiev / Dental Guru Academy
However, the volume of microbial contamination differs significantly. With a passive fit, biofilm is typically minimal, and any odor is usually slight and only noticeable upon removal. Conversely, with a poorly fitting prosthesis, significant biofilm accumulation can cause noticeable malodor. In any case, screw retention offers the advantage of retrievability, allowing removal for professional cleaning and maintenance of the prosthesis and underlying tissues. Patients should be encouraged to attend regular recall appointments (at least annually) for examination and professional hygiene.
What are the consequences if a non-passive restoration is forced into place?
Consider another crew retention example. The image shows significant inclination of both the implants and adjacent teeth. The restoration was seated, albeit with difficulty, achieving minimal visible gaps at the interface.

Forcing the restoration with internal stress resulted in bone resorption around one of the implants (left) YouTube / Dr. Kamil Khabiev / Dental Guru Academy
However, achieving this apparent fit came at the cost of inducing internal stress within the system. This indicates significant stress on the components and surrounding bone. This results in non-physiological, constant lateral loading of the peri-implant bone, even without occlusal function. The consequences, in the form of significant crestal bone loss around the implant, are clearly visible on the radiograph.
What if proximal contacts are aggressively adjusted to achieve seating?
Consider another clinical situation with difficulties fitting a single restoration. The posterior molar has tilted mesially into the long-standing edentulous space. The proximal surfaces are clearly not parallel.

Single restoration at different stages of fabrication and fitting – contact point between premolar and prosthesis YouTube / Dr. Kamil Khabiev / Dental Guru Academy
To achieve seating, the crown’s mesial proximal contact was modified by creating a concavity.

Incorrect (left) and correct (right) contact point between a restoration and adjacent natural teeth YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Now let’s explain what the problem is here. Normal contact between teeth allows the teeth to move relative to each other. And it is good when the tooth moves:
- The periodontium works well – the periodontal ligaments (PDL and the vasculature are stimulated
- The proximal surfaces self-clean when the teeth move relative to each other
Implant-supported restorations are immobile, but proper point contacts allow adjacent natural teeth to maintain their physiologic mobility relative to the fixed restoration.
In this case, the broad, concave contact area effectively splints the premolar to the immobile implant restoration, restricting its natural movement. This lack of physiologic stimulation can lead to PDL disuse atrophy. Paradoxically, the tooth might eventually become mobile, an open contact may develop, and in severe cases, the natural tooth could be compromised or lost over time, even though initially it might seem supported.
Let’s sum up the intermediate results.
- Utilize MUAs for multi-unit restorations whenever feasible. Direct-to-implant screw retention carries higher risks and technical challenges, particularly for bridges. Note that the problematic examples shown primarily involved direct-to-implant retention.
- If a framework or restoration exhibits misfit (e.g., visible gaps on radiograph, fails passive fit tests like the Sheffield test), it must be remade. Do not attempt to force it into place. Proceeding with a poorly fitting restoration inevitably leads to complications. Addressing the fit issue immediately prevents future failures and patient dissatisfaction.
Implant failure necessitates removal, potentially grafting, and a completely new surgical and restorative cycle.

Implant fracture – requires removal and replacement YouTube / Dr. Kamil Khabiev / Dental Guru Academy
- Consider implant systems with conical connections. They tend to offer better sealing and may be slightly more forgiving of minor prosthetic inaccuracies compared to flat-to-flat connections like internal hexes, potentially leading to better load distribution and reduced micromovement.
- Reject ‘compromise’ solutions from dental technicians if fit is inadequate. Modifications like improperly altering the mating surface of the interface (as shown below where a technician ground down the internal hex) should not be accepted.

The dental technician ground down part of the interface (internal hex), otherwise the restoration would not fit YouTube/Dr. Kamil Khabiev / Dental Guru Academy
This allowed the restoration to seat vertically but compromised the connection’s integrity. Note the left implant: the modified abutment interface barely engages the implant connection, essentially ‘hanging’ on the screw. The screw bears the entire load, as the stabilizing features of the interface are lost. Even if the screw holds temporarily, the large gap will accumulate debris and biofilm, leading to malodor and inflammation. Furthermore, micromovement of the improperly seated abutment transmits non-axial forces to the implant, increasing the risk of screw loosening, crestal bone loss, and potentially implant loosening over time. Eventually, the patient may present with a failed restoration or even a failed implant.
- Remember that microgaps exist even with clinically acceptable fits. Schedule regular recall appointments for examination, professional cleaning (including under pontics or around abutments), and reinforcement of oral hygiene instructions.
When is Screw Retention Clearly Indicated or Advantageous?
The cases described above can lead to a negative attitude towards screw retention. Actually this is not true. Here are the main scenarios for using screw retention, in which the likelihood of complications is minimal:
- When the vertical distance from the implant platform to the opposing dentition is less than 7 mm. We wrote about this in the first part. And under such conditions, no other type of retention will be reliable.
- Provisional restorations for immediate loading protocols. The material for provisional restorations is relatively soft plastic. And if there are problems with the fit, it can be easily ground or composite may be added if necessary. A plastic prosthesis will not be able to create excessive pressure. And there is no point in cement retention because it will have to be removed in a few weeks and a couple of months.

Provisional crown made of plastic YouTube/Dr. Kamil Khabiev / Dental Guru Academy
- Al- on-4 and All-on-6 restoration protocol. Only multi-unit abutments, both straight and angled, are used here.
- Significant inter-implant angulation. Multi-unit abutments allow you to compensate for significant angulation of implants relative to each other. The photo below shows an example of a bridge attached to implants placed at significant angles to each other.

Screw-retained bridge on MUAs, compensating for significant implant angulation YouTube / Dr. Kamil Khabiev / Dental Guru Academy
- Screw retention allows you to solve the problem of incorrectly placed implants relative to the orthopedic position. Examples in the photo below.

Full-arch restoration on 5 implants, one of which is placed between the positions of the teeth 6 and 7 YouTube / Dr. Kamil Khabiev / Dental Guru Academy

Screw retention supported by implants placed too palatally YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Of course, this is an attempt to correct the surgeon’s mistakes or cases where installing implants in parallel and in positions where there used to be natural teeth is impossible, but only screw retention can partially correct the situation.
Screw retention on multi-unit abutments: features
- It is necessary to use verification jigs. Without this, it is impossible to produce a prosthesis with a good passive fit. Cement does not compensate for minor inaccuracies.

- It is crucial to perform the Sheffield test when fitting a prosthesis or framework, especially for PFM restorations. This test involves securing one terminal screw and observing whether the entire structure lifts or gaps are visible.

An example of a framework that did not pass the Sheffield test: on the left abutment a gap is visible between the framework and the abutment base YouTube / Dr. Kamil Khabiev / Dental Guru Academy
While tightening the framework with a screw might eliminate the visible gap in such cases, it can introduce undesirable tension. The framework would then function like a stressed bowstring. This can lead to bone resorption or screw fracture. Therefore, a restoration failing the Sheffield test should be remade.
How to choose a retention method for a specific case
Barring specific contraindications, both screw-retained and cement-retained restorations can be successful in many situations. However, some general guidelines can aid in selecting the appropriate retention method.
Consider screw retention when:
- The interocclusal space (distance from the abutment base to the antagonist tooth) is less than 7 mm.
- The patient has a history of periodontitis. Even in successfully treated cases without current symptoms, minimizing cement exposure can reduce the risk of inflammation. For multiple unit restorations, a screw-retained bridge on multi-unit abutments can be advantageous.
- Restoring a complete edentulous arch using the All-on-4 protocol.
- Frequent adjustments and maintenance of the prosthesis and soft tissues are anticipated. Screw-retained restorations are retrievable, allowing for easy removal and reinstallation.
- Temporary prostheses are best retained with screws rather than cement.
Consider cement retention when:
- Esthetics are paramount, particularly in the anterior region. Cement-retained restorations eliminate screw access channels and the potential for color changes in composite filling the screw access.
- Most single-unit restorations are best cemented. Cement removal is generally straightforward, whereas placing a screw-retained crown on a tilted abutment can be challenging.
- Completely restoring the dentition with 8-10 implants using segmented bridges. Cement can compensate for minor manufacturing inaccuracies and discrepancies in implant angulation. Screw-retained restorations require high precision, typically achieved with CAD/CAM technology, which may not always be accessible. Furthermore, even the most precise manufacturing cannot eliminate the risk of gaps and biofilm formation within the implant-abutment interface.
There’s the controversial topic of implants with significant deviations from the arch form. Multi-unit abutments offer a standard, cost-effective solution for managing deviations with screw retention. Alternatively, custom abutments can correct for any reasonable deviation when using cement retention. Custom abutments entail higher expense, making it an individual decision.
We hope this information proves useful in your practice. Stay tuned for our next publications.
Disclaimer: Any medical or scientific information provided in connection with the content presented here makes no claim to completeness and the topicality, accuracy and balance of such information provided is not guaranteed. The information provided by XGATE Dental Group GmbH does not constitute medical advice or recommendation and is in no way a substitute for professional advice from a physician, dentist or other healthcare professional and must not be used as a basis for diagnosis or for selecting, starting, changing or stopping medical treatment.
Physicians, dentists and other healthcare professionals are solely responsible for the individual medical assessment of each case and for their medical decisions, selection and application of diagnostic methods, medical protocols, treatments and products.
XGATE Dental Group GmbH does not accept any liability for any inconvenience or damage resulting from the use of the content and information presented here. Products or treatments shown may not be available in all countries and different information may apply in different countries. For country-specific information please refer to our customer service or a distributor or partner of XGATE Dental Group GmbH in your region.
