Contents
Unfortunately, even the most experienced implantologists make errors, and complications can occur even if the surgical procedure was flawless. This article aims to provide examples and discuss techniques and methods that will help practicing surgeons avoid serious errors and reduce the risk of major complications. Most importantly, it covers how to rectify the situation if an error does occur. Quite often, patients come to practicing dentists with problems caused by less experienced colleagues, so the ability to correct such issues is equally important.
At What Stages Are Errors Possible?
- During treatment planning:
- Most often, the number of implants is insufficient, though there are cases of excessive implant density per unit of bone area.
- The distribution, angulation, and position of the implants may make it impossible to create a functional prosthetic structure.
- Restoration design. For example, a lack of segmentation between bridges; connecting the posterior and anterior sections of the restoration rigidly, where a long-span cross-arch restoration acts as a lever.
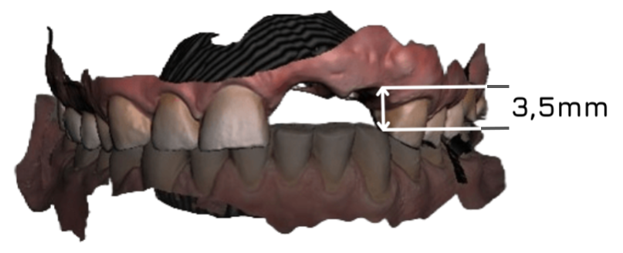
- Opposing and adjacent teeth position. Most often, there is a lack of vertical space between the implant platform and the antagonist tooth. In some cases, the situation can be resolved using multi-unit abutments (MUAs) and screw retention. For example, the MUA V-type from XGate Dental allows for prosthetic restorations even in challenging situations, as shown in the illustration below.
This solution relies on the low taper of the abutment. This series of abutments also features ultra-low sleeves with a height of just 0.5 mm above the abutment level.
However, it is not always possible to solve the problem this way. For example, regarding a single restoration, even multi-unit abutments with an ultra-low profile will not help, as they are intended primarily for multiple-unit splinted restorations.
- When planning soft tissue aesthetics, it is important to determine immediately whether the patient will require prosthetic gingiva or if a natural contour can be maintained, and whether there will be issues with the soft tissue seal.
- During prosthetics:
- Connecting implant restorations to natural teeth is generally contraindicated.
- Errors at the connection level (e.g., choosing a flat-to-flat connection, which is considered unreliable and problematic compared to conical or internal hex connections according to recent data).
- It is important to recognize signs of overloading and check the restoration before final retention.
- Errors in choosing between cement or screw retention.
- Failure to remove excess cement in contact with soft tissues.
- Lack of platform switching (or dual platform switching). This most often leads to gingival recession, as platform switching provides sufficient space for a robust connective tissue attachment, preserving not only the gingiva but also the crestal bone around the implant.
- The biocompatibility of the material and the soft tissue reaction to it.
- The shape of the abutment affects the fit and reliability of the restoration and is much more significant for long-term success than it might seem at first glance.
- Errors made during the manufacturing of crowns or bridges.
- Phonetic problems are often caused by prosthetic errors, most commonly regarding the contour of the restoration on the palatal aspect.
- Failure to disinfect abutments before installation. Surprisingly, some dentists do not sterilize abutments received from the dental laboratory.
- Other errors: transfer seating checks, abutment seating checks, and try-ins.
- Complications after prosthetics:
- Implant fracture.
- Abutment fracture.
- Fracture or loosening of retaining screws.
- Hygiene issues (the restoration is designed in a way that prevents the patient from performing adequate home care, regardless of effort).
- Problems with removable dentures.
- Fracture of the prosthesis.
- Excessive wear of components.
- Non-parallelism of abutments.
- Problems with bar-retained structures.
- Problems with mini-implants (bone resorption, gingival recession).
Implantation Planning Is the Key to Treatment Success
From the first visit to final rehabilitation, the patient goes through three main stages:
- Planning: This includes diagnostics, collecting all data on the patient’s general health, and establishing a treatment plan.
- Preparation: This includes the extraction of non-restorable teeth, bone grafting, soft tissue management, and the actual implant placement. Afterward, the protocol dictates whether to proceed with immediate loading or delayed prosthetics.
- Prosthetics: Options here include the design, fabrication, and delivery of a temporary prosthesis, or an immediate permanent one if a two-stage protocol was used, the implants are fully integrated, and the prosthetic structure is not overly complex.
Let’s look closer at the first stage. Its importance lies not only in collecting initial data but also in envisioning the final restoration. Therefore, it is crucial to plan the entire treatment process in consultation with the prosthodontist and, preferably, the endodontist. This collaboration dictates the number and positioning of implants, as well as the choice of abutments and retention type. This may sound surprising, but the prosthodontist should play a key role in the planning stage. The surgeon should execute the work as closely as possible to the prosthodontist’s vision.
If there is no clear plan and oversight from a prosthodontist, scenarios like the following become a reality (see image below).
In terms of implant integration and survival, the case may look successful surgically, with ample bone and soft tissue around the implants. However, creating a functional restoration on such a foundation is a challenging task. This leads to prosthetic failures like the one shown in the lower right slide.
The next important consideration is the number of implants. Some still believe that more is better. The photo below shows a relatively old case with an extremely dense placement of basal implants.

Moderate bone problems due to implants being too close together. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
This is not even the worst-case scenario. Because the body of basal implants is quite thin, there is enough bone tissue between them to maintain proper vascularization. However, prosthetic treatment in this case is incredibly difficult, and the prosthodontist may end up with a few gray hairs.
The next image shows a more serious problem: the number of implants is almost equal to the number of roots of the natural teeth. These are full-sized root-form implants with very little bone between them. One of the key rules has been violated: there must be at least 3 mm of bone between adjacent implants. Otherwise, vascularization is compromised, leading to inevitable inter-implant bone loss, followed by marginal resorption and peri-implantitis.

A major implantation error: too many implants with gaps much smaller than the acceptable 3 mm. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The other extreme is too few implants. In such cases, both the mechanical strength of the restoration and the implants themselves are compromised. The load on each fixture becomes excessive, leading to bone loss around the implant and the inevitable loss of the implants themselves.
The image below shows four implants in the upper jaw. All are long, providing an adequate contact area with the bone tissue, and the result is acceptable for the maxillary arch. Although the cantilevers on the upper jaw are slightly large, they are within an acceptable range.

An extremely low number of implants for full-arch restoration of the upper and lower jaws. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The lower jaw prosthesis rests on just three implants. This is not always an error; several studies confirm the viability of this design. However, not all specialists are prepared for such experiments.
In any case, both surgeons and prosthodontists must understand:
- 4 implants should be placed to form a trapezoid in the horizontal projection.
- 3 implants should form a triangle, similar to a tripod. Only such a structure will be stable and offer predictable long-term results.
In the clinical case shown above, the problem is not the three implants, but their arrangement and the massive cantilevers in the posterior sections.
Compare this with the next image. It features clear, stable triangles and almost no cantilevers. If the occlusion is optimized, this case has excellent long-term prognosis.

Optimal placement of implants in a triangular pattern, with implants spaced as widely as possible and minimal cantilevers. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The same cannot be said about the next case, where the entire restoration is supported by ONE implant.

A single-implant-supported design is an extreme solution and a highly undesirable configuration. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Surprisingly, even this design has a chance of serving the patient. This is because the patient has a removable denture secured to the gingiva. This acts as a safety mechanism; in the event of lateral or vertical overload, the removable denture will simply shift, leaving the underlying structure undamaged. The clinical picture in the last slide is the result of adequate planning given very limited resources.
In the next section, we will examine implant positioning errors, potential sinus complications (even if the sinus lift was performed correctly), compare the features of multi-unit abutments versus cement retention, and discuss many other points of interest to practicing dentists. See you in the next part of our review.
Disclaimer: Any medical or scientific information provided in connection with the content presented here makes no claim to completeness and the topicality, accuracy and balance of such information provided is not guaranteed. The information provided by XGATE Dental Group GmbH does not constitute medical advice or recommendation and is in no way a substitute for professional advice from a physician, dentist or other healthcare professional and must not be used as a basis for diagnosis or for selecting, starting, changing or stopping medical treatment.
Physicians, dentists and other healthcare professionals are solely responsible for the individual medical assessment of each case and for their medical decisions, selection and application of diagnostic methods, medical protocols, treatments and products.
XGATE Dental Group GmbH does not accept any liability for any inconvenience or damage resulting from the use of the content and information presented here. Products or treatments shown may not be available in all countries and different information may apply in different countries. For country-specific information please refer to our customer service or a distributor or partner of XGATE Dental Group GmbH in your region.