Contents
This article focuses on practical applications and specific case examples. Perhaps those who have not yet mastered the technique of full-arch restoration supported by 4 or 6 implants will find it necessary to undergo training and still include this service in their list. We also hope that experienced specialists will find valuable insights here.
Why are the full-arch on 4 or 6 implant protocols so popular?
First, let us recall that these protocols are not always the optimal option for a full-arch restoration. They were specifically developed for cases where the alveolar ridge in the posterior regions has undergone significant atrophy, making it impossible or too risky to place implants in the positions of the premolars and molars (teeth 5-7). Bone grafting procedures are associated with inherent risks, especially for patients over 70 years old.
That is why a protocol was developed in which the distal-most implants are placed at an angle. The idea is for the implant to be anchored in the relatively dense bone of the anterior jaw, while its restorative platform emerges more distally. This allows the final support for the prosthesis to be in the position of the first or second premolar, even when placing a vertical implant there is no longer feasible. As a result, the patient receives a restoration of a nearly full dental arch (most often extending to the first molars) without excessively long cantilevers.

Restoring a dental arch with angled abutments and tilted implants from Shutterstock
The key advantage of the full-arch protocol with immediate loading is speed. There is even a well-known illustration showing a patient who arrived at 9:00 a.m. with failing dentition and left with a functional prosthesis by 3:00 p.m.

Progressive concept of smile restoration in one day YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Of course, this day was preceded by a diagnostic and planning phase, including the fabrication of a temporary prosthesis, which took another couple of days. The point is that the technique of prosthetics on 4 or 6 implants has become so commonplace and well-established that patients began to specifically seek out this service even if they did not have direct indications for this protocol.
Which patients are indicated for restoration according to full-arch protocols on 4 or 6 implants?
The decision-making protocol developed by Dr. Paulo Malo is one of the simplest and most visual methods, and it is considered a classic.
| Bone tissue condition | Preview |
|---|---|
| No significant bone atrophy. No teeth remain, but bone volume is sufficient. There are no restrictions; 6-10 implants can be placed for any type of full-arch restoration. It is crucial to remember that the restoration should be fabricated as segmented bridgework. The full-arch protocol on 4 or 6 implants is not suitable here, as it is a compromise solution and should not be used when a classic restoration is possible. |  |
| Mild atrophy, but still sufficient bone tissue. It is better to use 6 implants, with the distal implants placed at a slight angle (e.g., 17°). |  |
| Moderate bone atrophy is a prime indication for the full-arch protocol on 4 or 6 implants. Distal implants are placed at an angle of 30-45°, providing the patient with a stable prosthetic foundation. |  |
| Severe atrophy. In such cases, distal implants may be placed using a trans-sinus technique. Zygomatic implants (e.g., Zygoma) are inserted from the premolar region and anchor into the zygomatic bone for bicortical fixation. IMPORTANT: Working with zygomatic implants requires qualification as a maxillofacial surgeon. |  |
| Advanced atrophy in the lateral sections, but sufficient bone in the anterior section for standard implants. This calls for a hybrid approach. Here, zygomatic implants are fixed in the zygomatic bone and, depending on the clinical picture, can be placed either extramaxillary or intramaxillary. |  |
| Near-complete atrophy of the alveolar ridge. All implants are zygomatic. In particularly complex cases, a custom-milled (often 3D-printed metal) subperiosteal zygomatic framework is manufactured. |  |
Most often, indications for the full-arch protocol on 4 or 6 implants are for elderly patients, typically 75 to 80 years and older, who:
- Have been edentulous for a long time and are long-term removable denture wearers, but their quality of life is no longer satisfactory. In such cases, implants are placed, and their existing removable denture can serve as a basis for a temporary fixed prosthesis. It is modified, reinforced, and converted to screw retention.
- Have lost their posterior teeth long ago and have only a few remaining anterior teeth. These are candidates for immediate implant placement and, if primary stability is sufficient, immediate loading. Here, a temporary prosthesis is fabricated from scratch based on scans and impressions that capture the bite.
Next, we will examine the specifics of both approaches in more detail.
Professor P.I. Brånemark once said, “No one should die with their teeth in a glass of water.” Doctors Brånemark and Paulo Maló are considered the pioneers of tilted implantation, a concept that was finalized and began to be widely used in the 1990s.
Regarding tooth loss statistics, the average person loses their first tooth between the ages of 35-40, and this data is for developed countries. Of course, at such a young age, it is easier to place a single implant and even perform guided bone regeneration (GBR) if necessary, without fearing significant complications.
With age, the situation deteriorates, and by 65-70, people on average have lost most or all of their teeth. While there are pleasant exceptions, implantologists frequently work with elderly patients in need of full-arch restorations.
But while at 60-70 years old people often still have enough bone to place 8-10 implants, by age 80, very little may be left of the alveolar ridge. The loss of vertical height is especially noticeable in the mandible. When a removable denture is taken out, you may see the so-called “witch’s chin” appearance.

Example of bone loss in elderly patients with complete edentia (“witch’s chin”)
In conditions of severe bone deficiency, the full-arch protocol on 4 or 6 implants or even the placement of zygomatic implants are often the only viable options for dental restoration.
Risks associated with tilted implant placement and the use of angled abutments
It is evident that an angled abutment on a tilted implant will experience greater biomechanical loads compared to a straight implant and abutment. Many clinicians are concerned about this issue, as almost everyone has experienced cases of cement failure, screw loosening or fracture, and other problems associated with angled components.
Studies have addressed this. We have an article on our website summarizing one such study: “Screw Retention on Multi-Unit Abutments: What Happens to Implants, Screws, and Bone Tissue Under Vertical and Horizontal Loads” which confirms that the greater the angle, the higher the load on the superstructure.
However, when comparing the risks, replacing a broken screw or even an abutment is far simpler than undergoing a large-scale and risky bone grafting operation.
Furthermore, studies have shown that distally placed implants are always subjected to greater loads compared to mesially placed ones, regardless of their angulation or the total number of implants. And yes, a tilted implant experiences greater stress than a straight one, but the length and bone-to-implant contact (BIC) area of a tilted implant are also greater.
Therefore, most tilted implants serve successfully for 5-10 years or more.

Problems like mucositis and peri-implantitis arise almost independently of the implant’s angulation. They are more commonly associated with errors in prosthetics or poor oral hygiene. For example, an ill-fitting prosthesis with internal stresses will lead to bone resorption around the implant, inflammation, and so on. But this is a topic for a separate article.
So, while there are risks associated with tilted implant placement and the use of angled abutments, they are less significant than the risks and potential complications of bone grafting in this age group. Therefore, in this specific niche, the use of 30° and even 45° angled abutments is a justified risk.
How to choose material for a prosthesis
First and foremost, you need to consider the materials of the opposing dentition. It often happens that only one arch needs to be restored. For example, a patient has had an upper prosthesis for a long time, made of, say, porcelain-fused-to-metal (PFM). If you make the lower prosthesis from zirconia or also from PFM, problems will arise. Both are hard and brittle materials, and regular occlusal contact will likely lead to chipping or fractures on one or both prostheses.
Therefore, it makes sense to fabricate the lower prosthesis, for example, on a titanium bar with a composite veneering. Yes, the composite wears down faster, but even heavy occlusal impact between PFM and composite will not cause fractures.
There are also other material combinations that do not lead to premature wear of the restoration. In general, when choosing a material, we have two risk zones:
- Functional: Risk of mechanical failure or the inability to restore 100% of chewing function.
- Aesthetics: The prosthesis should look natural without damage or discoloration.
The clinician needs to find a balance and evaluate each case individually.
Orthopedic and anatomical rationale for prosthetics with tilted implants
Look at the illustration below; it clearly shows the relationship between the implant’s angle of inclination and the length of the cantilever in the posterior region. The first example is the mandible.

Reducing the cantilever length of the prosthesis by increasing the implant’s angle of inclination (mandible) YouTube / Dr. Kamil Khabiev / Dental Guru Academy
A long cantilever (more than 10 mm), especially a distal one, is one of the most serious problems in prosthetics. It acts as a lever, creating a constant force that can overload the anterior implants.
There are two ways to reduce the cantilever length:
- Restore a shortened dental arch, for example, terminating at the first or second premolars.
- Increase the angulation of the distal implants, for example, from the standard 30° to 45°.
The illustration shows that:
- At an angle of 15-17°, the cantilever length will be at least 15 mm.
- If the angle is 30°, the cantilever is reduced to 9 mm.
- And if you increase the angle to 45°, the cantilever length will be only 7.5 mm.
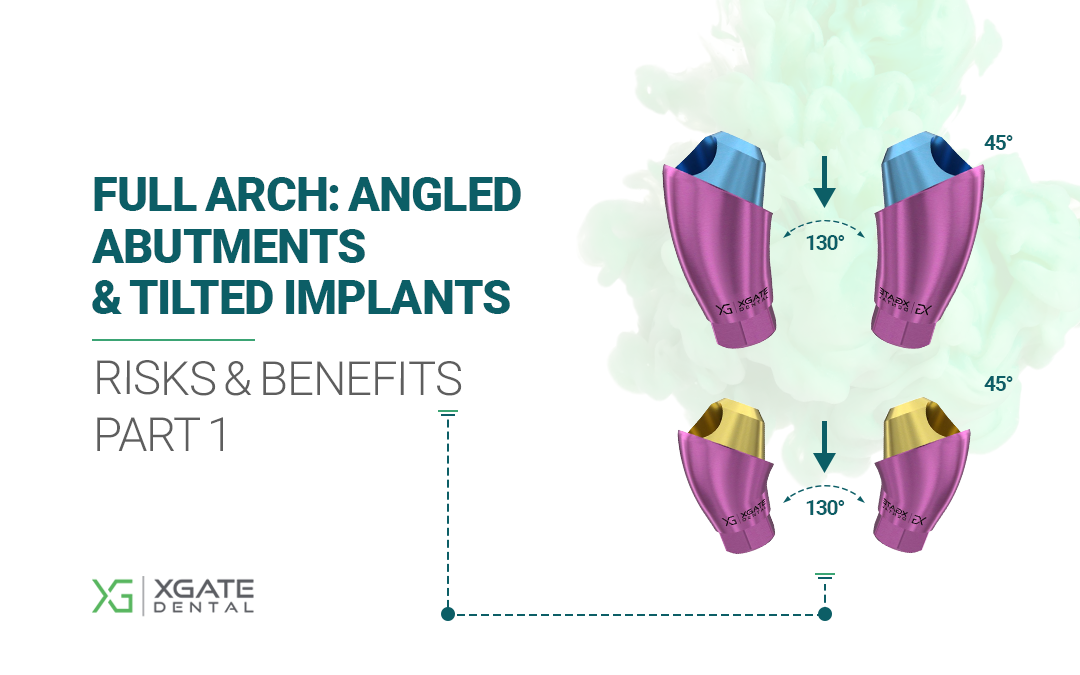
Many have 45° angled abutments, but not all. XGate has such items, see the illustration below. Pay attention to the color of the coating, it is as close as possible to the color of the living gum.

45° Angled MUA by XGate Dental
Reducing the cantilever length decreases the load on the bone surrounding the implants. Here we observe a multi-faceted process. On one hand, increasing the angulation increases the load on the abutment and its retaining screw. On the other hand, we shorten the cantilever, reducing the lever arm and thus decreasing the load on the bone around the implant.
A similar picture is observed in the maxilla, albeit with a slightly smaller cantilever effect.

Reducing the cantilever length of the prosthesis by increasing the implant’s angle of inclination (maxilla) YouTube / Dr. Kamil Khabiev / Dental Guru Academy
It is also worth mentioning studies that have looked at mandibular rotation and flexion. Dr. Hylander studied macaques (American Journal of Physical Anthropology, 1994), and Dr. Marx investigated the biomechanics of the human jaw.
The key takeaway for us is that the mandible flexes and twists slightly during chewing movements, primarily due to the action of the pterygoid muscles.

The principle of mandibular deformation and its implications for prosthetics supported by anteriorly placed implants YouTube / Dr. Kamil Khabiev / Dental Guru Academy
For surgeons and prosthodontists, this has the following practical implications:
- Full-arch restorations should be segmented into separate bridges whenever possible. Fabricating a prosthesis from second molar to second molar as a single, monolithic structure is a poor decision. Such an arch will be subjected to twisting and bending forces, and the prosthetic material is not as flexible as living bone. This conclusion aligns with standard protocols, where a restoration on 8-10 implants is divided into 3-4 bridges. The posterior segments (premolars/molars) are always separated from the anterior segment. For the anterior sections:
- On the mandible, it should always be a solid piece.
- On the maxilla, it can sometimes be divided at the central incisor, depending on the state of the median palatal suture. In some adults, this suture retains slight mobility. If the suture is firmly fused, division is not necessary.
- If the entire restoration is supported by implants concentrated in the anterior part of the jaw, problems associated with mandibular twisting and flexion are minimal or non-existent. This is another advantage of the full-arch protocols on 4 or 6 implants with this specific implant arrangement.
Standard diagram of a fixed prosthesis supported by 4 and 6 implants (maxilla)
These diagrams are based on the source: ITI (Capelli, Testori et al. 2007-2008).

First, let’s look at the prosthesis diagram for the full-arch protocol on 4 implants, where two implants are placed vertically, and two distal implants are tilted at an angle of 17° to 45°. This allows for bypassing anatomical limitations and reducing the cantilever length.

Fixed prosthesis diagram for the full-arch on 4 implant protocol YouTube / Dr. Kamil Khabiev / Dental Guru Academy
This setup allows for restoring the dental arch up to the second premolars (5s). While not ideal, it is a significant improvement over removable dentures.
The diagram for the full-arch on 6 implant protocol looks more promising. Here, four implants are placed vertically, and two distal ones are tilted. The additional pair of implants allows for restoring the dentition to the first molars (6s). This provides nearly 100% restoration of chewing function, but placing 6 implants is not always possible.

Fixed prosthesis diagram for the full-arch on 6 implant protocol YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Advantages of tilted implants
Let’s summarize the advantages of placing implants at an angle:
- Increased primary stability due to a larger bone-to-implant contact area. Primary stability is critical for immediate-load restorations.
- Reduced cantilever length of the prosthesis by increasing the anterior-posterior (A-P) spread between the support points. The tilt allows the implant’s restorative platform to be positioned further from the adjacent implants, leading to more even load distribution.
- Avoidance of complex and risky bone grafting operations, such as guided bone regeneration (GBR) on the mandible and sinus lifts on the maxilla. It also reduces the risk of damaging the mandibular nerve and other vital anatomical structures.
Why is guided surgery necessary for implant placement?
The accuracy of implant placement, especially at an angle, is critical for long-term success. Just as a plane deviating its course by a few degrees will end up in a different city, an improperly placed implant creates major prosthetic challenges. Achieving a good passive fit for the final restoration becomes extremely difficult.
Therefore, planning the surgery on virtual jaw models and placing implants using a surgical template is very important because:
- The risk of errors during implant placement is minimized, making it easier for the prosthodontist to fabricate a prosthesis that fits perfectly without adjustments or modifications.
- The result is always predictable, and the patient receives exactly the restoration that was planned and discussed.
- The invasiveness of the surgical procedure is minimized. This means less pain, swelling, and faster healing, with the risk of complications reduced to a minimum.
Although many surgeons use templates only for complex cases, we do not advocate working without surgical templates but rather aim to convey the logic of experienced colleagues. This approach is based on the idea that it is extremely important for the surgeon to develop tactile skills and feel the feedback from the bone. Unfortunately, even the most modern diagnostic methods do not allow for a 100% accurate determination of bone density in a specific area. Therefore, it is important to feel how the drill advances, whether the irrigation is sufficient, and if the implant is seated evenly.
These skills can and should be acquired on practice models, not on patients, especially those with bone deficiencies. You can use wooden blocks of different densities or plastic training models of jaws to practice drilling and placing implants. Yes, you will have to sacrifice several burs, but as experienced colleagues say, it is worth it.

Study model of a jaw with placed implants and an R2Gate surgical template YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Since the full-arch protocols on 4 or 6 implants involve an edentulous jaw, surgical templates with bone or mucosal fixation are used. Let’s look at a specific example.
- First, an accurate 3D model of the patient’s jaws is required. This is achieved by combining CBCT and optical scan data.

Virtual model of the patient’s lower jaw YouTube / Dr. Kamil Khabiev / Dental Guru Academy
- Then, in a program like Exocad, the future dental arch is designed.

Virtual model of the future dentition YouTube / Dr. Kamil Khabiev / Dental Guru Academy
- The model with the planned teeth is imported into the software where the surgical template will be designed. The positions of the implants and the future restoration are merged. After necessary adjustments, a navigation template is created for the precise placement of the implants.

Aligning the planned restoration with the dental implant placement sites YouTube / Dr. Kamil Khabiev / Dental Guru Academy
- The digital file is sent to a 3D printer, where the surgical template itself is printed, such as the one in the picture below with bone fixation.

Surgical template for placement of 4 implants from Shutterstock
A well-stabilized surgical template ensures precise implant placement in terms of both depth and angulation.
Furthermore, there are fully guided templates that also control the rotational position of the implant’s internal interface. This is crucial for ensuring that angled abutments are oriented exactly as planned on the virtual model.

A fully guided surgical template controls not only the depth and angle of implant insertion but also the rotational position of the internal interface. A hand instrument for final implant seating has colored markers; when the green marker appears in the template slot, it means the implant is perfectly positioned YouTube / Dr. Kamil Khabiev / Dental Guru Academy
IMPORTANT! When using a surgical template, more intensive irrigation is needed, as the risk of overheating the bone is slightly higher, especially in the anterior mandible, where the bone is densest (D1-D2).
Surgery and prosthetics in the full-arch protocol on 4 or 6 implants: why one is impossible without the other
Let’s explore how dentists are trained and what models are used. We’ll take one of the most common cases: a patient who has been a long-term removable denture wearer but is no longer satisfied with their quality of life.

Model of a jaw with a tissue-supported removable denture YouTube / Dr. Kamil Khabiev / Dental Guru Academy
This is what an edentulous jaw of a long-term denture wearer looks like. The model is made of materials that accurately imitate both soft and hard tissues.

Edentulous jaw model for training students and young specialists YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Since both the upper and lower dental arches will be created from scratch, it is necessary to plan and mark the position of the future teeth. One method is to use a positioning guide for the dental arch to mark the central points of the crowns. After this, an incision is made along the crest of the ridge, and a flap is reflected to provide access to the bone.

Positioning template YouTube / Dr. Kamil Khabiev / Dental Guru Academy
If we remove the soft tissue imitation, we are left with a model of the bare jaw. It’s clear that in the anterior section, the alveolar ridge is still suitable for implantation, unlike in the posterior sections. There is also a typical problem for such patients: the alveolar ridge in the anterior section is much higher than in the lateral sections.

Bare jaw model for training implant placement according to the full-arch protocol on 4 or 6 implants YouTube / Dr. Kamil Khabiev / Dental Guru Academy
This means that an alveoloplasty (ridge reduction) must be performed to level the alveolar ridge. This is especially important if immediate loading is planned. The second indication for ridge reduction is a very thin, knife-edge ridge.
IMPORTANT! When placing implants after an alveolar ridge reduction, it is important to remember that the dense cortical layer is no longer present. The implant is placed into the cancellous bone. As a rule, the drilling protocol is modified; it may not be necessary to use the widest diameter drill or to countersink the osteotomy. However, the clinician determines this for each specific case.
Next, we determine the implant placement sites and transfer these markings to the model. At the training stage, it is also necessary to mark the area where the mandibular nerve is located. A surgical marker or biological ink is used for marking on bone tissue.

Marking the implant placement sites for a full-arch protocol on 4 or 6 implants YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Next, we proceed to the pilot drilling. In this case, drilling is done freehand without a navigation template, specifically to develop manual skills and a tactile feel for bone.

Pilot drilling to prepare the osteotomy for implants YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Next, we place the vertical implants in the incisor positions.

The first two implants have been placed in the training model YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Placing tilted implants is somewhat more complicated. It’s not enough to simply insert them into the bone; a recess must be prepared to allow for the proper seating of the angled abutments. One method is to place cover screws in the implants and carefully perform an osteoplasty around them with a round bur.

All four implants have been placed. In the area of the tilted distal implants, bone has been recontoured to allow for the passive seating of angled MUA abutments. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Next, we install the multi-unit abutments, torquing them to 30-35 Ncm. There are even special carriers and drivers for this. The carriers are designed to break off when the required torque value is reached.

Installation of multi-unit abutments using special break-away carriers with a fixed torque value (they shear off when the required force is reached) YouTube / Dr. Kamil Khabiev / Dental Guru Academy
One of the advantages of MUAs is that they are installed on the day of surgery and are not disturbed thereafter. This promotes healing. A key advantage of screw-retained solutions is the ease of achieving a passive fit, because the entire prosthetic interface is supragingival and clearly visible. The picture below shows the final result with all 4 MUAs installed.

Study model with installed implants and multi-unit abutments YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The next step is to reposition the soft tissues. At this stage, we also place either healing caps or scan bodies on the multi-units, which is necessary for taking an impression.

 Preparing for the next stage: repositioning the flap and placing healing caps YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Preparing for the next stage: repositioning the flap and placing healing caps YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Next, we suture the soft tissues. Large, simple interrupted sutures are placed first to secure the main sections of the flaps.

Preliminary flap stabilization with large sutures YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Then, we adapt the gingiva with a continuous horizontal mattress suture so that it is pulled snugly around the healing abutments.
At this point, the surgical stage is complete, and we proceed to prosthetics. The patient’s existing removable denture, modified for screw fixation, will be used as the temporary prosthesis.

Beginning the modification of a removable denture for use as a screw-retained temporary prosthesis YouTube / Dr. Kamil Khabiev / Dental Guru Academy
First, a pickup impression is made using silicone to capture the implant exit points.

Impression marking the implant locations on the old removable prosthesis (educational material) YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Afterward, the dental technician drills holes exactly in the center of each implant axis. In this example, the removable denture will not be reinforced, but there is a risk that in a couple of weeks, when the pain and swelling subside, the patient may forget and break it.

Marking for future screw access channels for fixing the prosthesis on multi-unit abutments YouTube / Dr. Kamil Khabiev / Dental Guru Academy
There are different methods to solve this problem. For example, Easy Bar is a kit of reinforcing links for such cases. Links of the required length are selected and fixed on temporary cylinders. Reinforcing links can be straight, as in the picture below, or curved, which are often easier to work with.

Reinforcing links for strengthening plastic dentures YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The reinforcing framework is assembled intraorally and fixed with autopolymerizing acrylic resin or a similar material compatible with the denture base acrylic.
Let’s return to our example. After marking, the dental technician removes the excess flange from the prosthesis. Previously, this part of the denture increased the area of contact with the mucosa, but now with implant support, this flange will interfere.

 Marking and removing the excess flange from the removable denture YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Marking and removing the excess flange from the removable denture YouTube / Dr. Kamil Khabiev / Dental Guru Academy
We proceed to prepare the most important area, marked in the picture below. This is the intaglio surface that contacts the mucosa. It should be shaped very carefully, without any concavities or undercuts, to ensure it is cleansable and does not accumulate plaque.

Marking the contact area of the temporary prosthesis with the mucosa – this surface must be thoroughly smoothed, with no irregularities or undercuts YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The dental technician then widens the holes, and the temporary prosthesis is ready for try-in.

Holes widened for fitting the prosthesis onto temporary cylinders YouTube / Dr. Kamil Khabiev / Dental Guru Academy
At this time, temporary cylinders are placed on the multi-unit abutments. They are long because they are designed to be trimmed down. During the fitting process, the dental technician will cut off the excess. It is on these cylinders that reinforcing links are typically fixed to increase the strength of the temporary prosthesis. But in our example, the prosthesis is relined without reinforcement.

Sleeves for securing temporary prosthesis YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The surgical site is isolated with a rubber dam to prevent saliva and blood from contaminating the prosthesis during the reline procedure.

Placing a rubber dam before relining a prosthesis YouTube / Dr. Kamil Khabiev / Dental Guru Academy
We place the prepared prosthesis over the cylinders and stabilize it with a small amount of autopolymerizing acrylic resin.

 Preliminary attachment of a temporary prosthesis to cylinders YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Preliminary attachment of a temporary prosthesis to cylinders YouTube / Dr. Kamil Khabiev / Dental Guru Academy
While this process is straightforward for the mandible, where the old denture rests on the mucosa and is easy to control, securing a maxillary prosthesis requires a different approach. It is best to make a silicone index (putty key) before the surgery to ensure the prosthesis is easily seated in the desired position during conversion.
The prosthesis is removed together with the cylinders, the rubber dam is taken off, and the dental technician fills the space between the cylinders and the body of the prosthesis with autopolymerizing acrylic resin. In this case, it looks a little messy because this is a student’s work. But this is not a major issue, as the prosthesis will be trimmed and polished.

Securing the cylinders in the body of the prosthesis using autopolymerizing acrylic resin YouTube / Dr. Kamil Khabiev / Dental Guru Academy
In the final stage, all excess material is removed, the surfaces are polished, and the work takes on a finished look.

 Polished denture ready for delivery YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Polished denture ready for delivery YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Yes, this is a student project, and in addition to the lack of reinforcement, one could also critique the length of the distal cantilevers. While such cantilevers might be acceptable for a permanent prosthesis, for a temporary prosthesis made of acrylic, it is better to shorten it immediately after the distal implant.
This is how the final work looks secured on the model of the oral cavity. A significant portion of the necessary skills for this procedure—involving the surgeon, prosthodontist, and dental technician—is acquired on such models.

The finished educational project is secured on the jaw model YouTube / Dr. Kamil Khabiev / Dental Guru Academy
In the next part of the article, we will consider a real clinical case of single-stage full-arch implantation with immediate loading. Stay tuned for the next publication.
Disclaimer: Any medical or scientific information provided in connection with the content presented here makes no claim to completeness and the topicality, accuracy and balance of such information provided is not guaranteed. The information provided by XGATE Dental Group GmbH does not constitute medical advice or recommendation and is in no way a substitute for professional advice from a physician, dentist or other healthcare professional and must not be used as a basis for diagnosis or for selecting, starting, changing or stopping medical treatment.
Physicians, dentists and other healthcare professionals are solely responsible for the individual medical assessment of each case and for their medical decisions, selection and application of diagnostic methods, medical protocols, treatments and products.
XGATE Dental Group GmbH does not accept any liability for any inconvenience or damage resulting from the use of the content and information presented here. Products or treatments shown may not be available in all countries and different information may apply in different countries. For country-specific information please refer to our customer service or a distributor or partner of XGATE Dental Group GmbH in your region.