Contents
In this article, we discuss the general principles of planning and treating patients with complete edentulism or remaining hopeless teeth. This material is intended for both novice and experienced dentists, regardless of the implant system used.
Why is it important to master the Full-Arch on 4/6 technique?
Practicing dentists frequently encounter patients with total tooth loss or a terminal dentition with 4–8 hopeless teeth remaining. Increasingly, patients request immediate results: they want to “go home with teeth” rather than wait several months while enduring the discomfort of removable dentures. The Full-Arch on 4/6 protocol was developed specifically for these cases.
It is efficient, cost-effective, and provides immediate aesthetic restoration and functional recovery (partial or complete) within a few months. Furthermore, the strategic selection and positioning of 4–6 implants often eliminate the need for complex bone grafting. This is crucial because these patients almost always present with bone deficiency or localized defects.
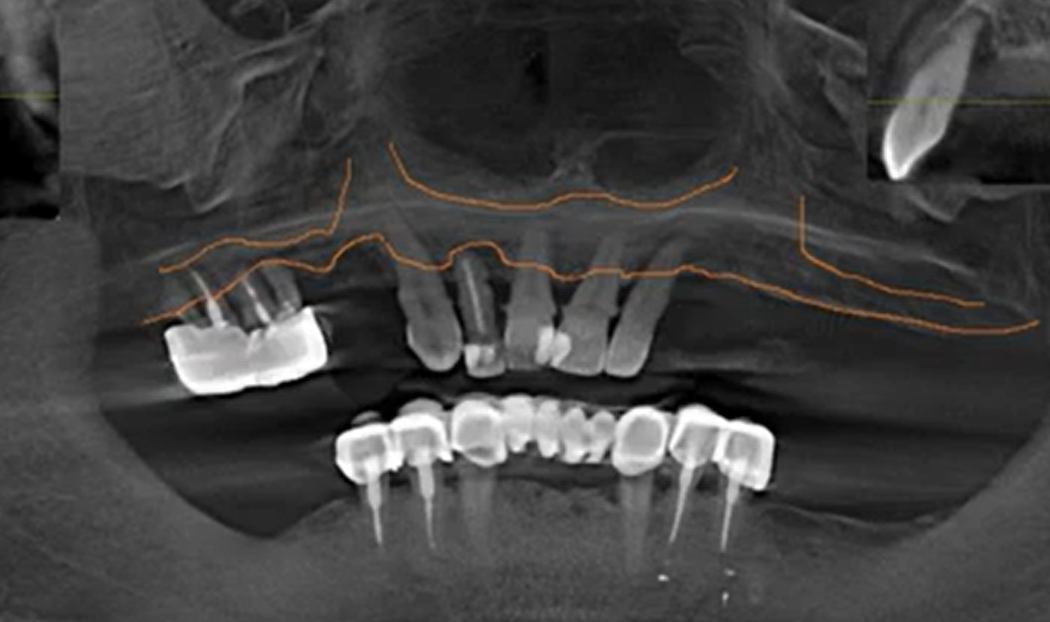
An example of a clinical situation with hopeless teeth and bone deficiency. The Full-Arch on 4/6 protocol helps avoid risky bone augmentation surgeries. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
Consider a patient with severe periodontitis, mobile teeth, and significant bone loss in the maxilla. A classic (delayed) protocol would require multiple bone grafting surgeries, each carrying specific risks. While a restoration supported by 8–10 implants is often considered more “reliable” (as it eliminates cantilevers and allows the arch to be divided into segments), the Full-Arch on 4/6 protocol offers a streamlined alternative. In this protocol, the arch typically ends at the first molars, often utilizing distal cantilevers.
The primary advantage is time. In a classic protocol, the patient might not receive a functional restoration for 12–18 months. Many patients, particularly the elderly or those with comorbidities, are not prepared for such an extended treatment timeline.
The Full-Arch on 4/6 technique offers “functional sufficiency” while minimizing surgical interventions. Additionally, because this protocol utilizes screw retention, maintenance and prosthetic replacement are simplified. A screw-retained bridge is easily removed for hygiene or repair, unlike cement-retained prostheses.
Immediate implantation: advantages and risks
Just 10–12 years ago, many surgeons discouraged this practice and, in most cases, followed a deferred protocol. As a reminder, this refers to cases where one or more teeth are extracted and an implant is placed immediately afterward. Since the topic of our article is total restorations, we are discussing the removal of all remaining teeth and the placement of the required number of implants. Not all implants will necessarily be placed in the sockets of extracted teeth; the position of the implants is determined by the treatment plan, and several implants may be placed in areas where teeth were lost long ago.

A typical situation in which the remaining teeth are extracted and some implants can be installed in the sockets of recently extracted teeth. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
Immediate implantation is now considered a standard procedure, and if there are no contraindications, doctors strive to place the implants immediately. Afterward, two scenarios are possible:
- Immediate loading: Placement of a temporary prosthesis, which corresponds to the Full-Arch on 4/6 technique.
- Postponed prosthetics: Waiting 1.5–3 months until the completion of the osseointegration process.
- The vestibular and lingual/palatal walls are often still intact, reducing the need for complex and risky bone grafting.
- It is easier to preserve or even increase the volume of attached gingiva, especially if a connective tissue graft is performed simultaneously.
- The overall number of surgical interventions is reduced. This is a significant advantage, as even minor surgery carries a risk of complications.
- The overall treatment time is reduced. The patient receives a permanent prosthesis within 3–5 months. If primary stability and the overall clinical situation allow, the patient can leave with a temporary prosthesis on the day of surgery.
Of course, there are contraindications to immediate implantation, but there are not many of them and, fortunately, they are quite rare.
Examples of successful immediate implant placements followed by prosthetic restoration are shown in the images below. As can be seen, the angled implants also integrated well and the restoration is sound.

An example of restoration on implants placed immediately after tooth extraction. YouTube/ Dr. Sergey Rozhnov /sergiodontolog
While contraindications to immediate implantation exist, they are relatively rare. Angled implant placement also deserves special attention. Although the load is distributed unevenly and the abutment and retention screw experience greater stress compared to axial placement, an angled implant allows the clinician to:
- Overcome anatomical limitations (e.g., local bone deficiency or proximity to the mandibular nerve).
- Avoid sinus lift—the risk of complications with sinus lift is among the highest in implant dentistry.
- Reduce the overall cost of treatment for the patient.
Immediate prosthetics using the Full-Arch on 4/6 method – conditions for long-term success
While we can use implants to close localized defects (such as incisors lost to trauma), our primary interest here is full-arch dentures supported by 4/6 implants. The patient immediately goes home with a temporary denture, which can last from several months to a year and a half.
For the success of the Full-Arch on 4/6 protocol, the following are essential:
- Comprehensive Research and Planning: Thanks to digital technologies and programs like Exocad®, planning can be completed in a single day. It is crucial that both the surgeon and the prosthodontist (restorative dentist) are involved. If the specialist does not perform both roles, the prosthodontist should have the final say in the treatment plan.
- Adequate Primary Stability: The simplest method of checking stability is the implant insertion torque. Below is a table showing the appropriate strategy for different torque values:
| Primary torque | Tactics | Prognosis |
|---|---|---|
| 0-10 Ncm | Place a larger-diameter implant with acceptable torque. Soft tissue capping and suturing are for a delayed protocol only. | Bad – if the implant is not reinstalled. |
| 10-30 Ncm | Fixation of the cover screw and suturing of soft tissues. | Satisfactory, but only with a delayed protocol |
| 30-40 Ncm | Fixation of a healing cap. | Good – early loading is possible if the stability according to ISQ is >70 |
| 40-50 Ncm | Placement of an abutment (temporary or permanent) and a temporary prosthesis is allowed. | Excellent without restrictions |
| More than 60 Ncm | The implant is removed, the osteotomy is widened, and the implant is reinstalled with a force of no more than 50 Ncm. | Bad – if the implant is not reinstalled. An exception is the installation of cancellous implants in loose bone (D3-D4), where high torque may not indicate bone injury. |
However, torque is still not always a reliable indicator. A more accurate indicator is the Implant Stability Quotient (ISQ), measured using resonance frequency analysis. Of course, there are limitations that affect accuracy, including bone type (D1–D4), implant length and diameter, and implantation depth. However, these indicators are more reliable, especially when measuring secondary stability.
- ISQ less than 55–60: Low stability, risk of failure.
- ISQ 60–70: Acceptable stability, suitable for early loading.
- ISQ 70–85: High stability, safe for immediate loading.
- Equally important is the placement of implants in the correct orthopedic position, which is facilitated by the use of surgical guides. In the digital age, custom-made surgical guides can also be created very quickly.
- A high-quality designed and manufactured prosthesis. If a patient has been edentulous for a long time, reproducing a proper bite is a challenging task.
Let’s explore these and other aspects of immediate implantation in more detail below.

One of the options for creating a full-arch restoration: using intraoral welding YouTube/ Dr. Sergey Rozhnov /sergiodontologist
Selecting the optimal number of implants: 4 or 6
Each clinical case is individual, but there is a general pattern, as shown in the image below. Here, six implants were placed in the maxilla and four in the mandible.

An example of restoration of both dental arches: the dentures are reinforced, the maxilla has 6 implants for better load distribution in the loose bone, the mandible has 4 implants, which is sufficient, since the mandible bone is denser. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
Such decisions are based on the fact that the bone tissue of the maxilla is not as dense as that of the mandible. Often, even in the anterior region, the density is D3, while in the posterior region, it is D4. However, proper selection of implant length, thread aggressiveness, and angled placement of distal implants allows for the creation of a stable structure even with four implants. We will discuss the selection of the number of implant lengths and diameters in more detail in the next part of this series.
What types of prostheses are used for the Full-Arch on 4/6 protocol?
The Toronto Bridge remains the gold standard—it immediately covers damaged gingiva and looks aesthetically pleasing. Its strength, thanks to its metal frame, ensures a service life of 10 years or more, which is a very good indicator.
Besides its simplicity and strength, the Toronto Bridge has other advantages:
- Easy to adjust or repair the cladding (ceramics or composite).
- Softer chewing surface (composite provides shock absorption compared to zirconia).
- Lighter weight (less stress on implants and TMJ).
- Lower price than milled zirconia.
Despite their simplicity and affordability, Toronto Bridge prostheses do have some disadvantages:
- The lining wears over time and requires maintenance every 1.5–2 years.
- service life is shorter than zirconia (usually up to 15 years).
With the development of digital technologies, particularly CAD/CAM, a growing share (around 40%) is made up of solid-milled zirconia dentures. They have the same shape and appearance, namely crowns and artificial gingiva, but the restorations made of zirconia:
- Are almost not subject to wear and tear, which means there is no need for repairs and adjustments.
- Zirconia retains its color, there is no effect of pigment absorption and loss of aesthetics.
- Durability – if there is no damage, the service life of a zirconia prosthesis is unlimited.
In general, a zirconium dioxide prosthesis is positioned as a premium solution, but it does have some disadvantages:
- Heavy weight and a very hard surface – when the jaws close, a noticeable impact load occurs, so many doctors strive to increase the number of supporting implants
- A zirconia prosthesis requires greater precision and a passive fit compared to PFM. Despite its hardness and wear resistance, zirconium dioxide is less able to withstand bending and torsional loads and can crack. However, digital planning and manufacturing solves the accuracy issues.
- If a chip or crack does occur, repairing the prosthesis is very difficult; most often, a new prosthesis has to be made.
- Not all patients can afford it due to its high price.
Planning the final restoration – “From end to beginning”
The success of future restoration begins with analysis:
- Bone volume and density analysis.This is important for choosing the correct positions for implant placement. Most often, patients have bone defects, a thin alveolar ridge, irregularities, cysts, etc. A typical picture is a height difference between the anterior and posterior jaws. Typically, the anterior teeth in both jaws last longer, and the alveolar ridge is higher than in the posterior jaws.
Conventionally, three zones of analysis can be distinguished, see the picture below:
- Frontal section – highlighted in blue
- Masticatory group – highlighted in red
- Canine-premolar group – highlighted in green
The image above shows an uneven alveolar ridge in the anterior region, as well as a noticeable bone deficiency in the masticatory zone of the first quadrant. This means that after tooth extraction, a bone reduction in the anterior region will be necessary.
The image above shows a typical scenario. Preliminary analysis is critical for protocols with a limited number of implants.
Now let’s return to the question of why the planning stage should be conducted in collaboration with the prosthodontist. Because the prosthodontist thinks in terms of the finished restoration, literally “seeing” the finished prosthesis and working backwards. For example, the prosthodontist sees that the patient is a large man with strong jaws. They understand that long cantilevers are a poor solution in this case. So, together with the surgeon, they determine the position and angle of the implant placement so that the cantilever length is no more than 10 mm.
How to choose the optimal number of implants in Full-Arch on 4/6 protocols
Here we need to take into account both the anatomical features of the patient and the condition of the bone. For example, there are standard recommendations for the distance between implants and the length of the cantilever sections of the prosthesis:
- The optimal distance between implants is 1.5-2 cm.
- The length of the cantilever sections is no more than 14 mm.

An example of the optimal placement of support points and the normal length of the cantilever sections of the Full-Arch prosthesis. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
But this does not take into account the anatomical features of the patient and the density of bone tissue in different areas. You cannot apply the same approach to a large patient with wide, massive jaws and to a small, thin-boned person.For people with medium and small jaw sizes, 4 implants may be sufficient for a fully effective restoration.
For larger patients or those with bone density issues, the number of implants is increased. It doesn’t necessarily have to be six implants; the image below shows a solution with five implants. This is quite effective in terms of load distribution.
An example of placing 5 implants for optimal load distribution – the implants are installed immediately after tooth extraction and ridge reduction, and are placed in dense bone between the sockets of the extracted teeth, which increases the primary stability of the Full-Arch. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
- Analysis of interocclusal distances. In cases of complete edentulism, the bite block method remains the most accurate method today. However, anthropometric measurements help make the model more accurate and avoid excessive or insufficient height of future prostheses.


Basic techniques for recording interocclusal height for creating future prostheses, top to bottom: anthropometric measurements, working with a Full-Arch bite block. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
If there are remnants of teeth or old prostheses, the task is easier, but the volume and complexity of the work remain high. In the images below are several examples of restorations.

A PFM mandible prosthesis supported by 4 implants – optimal height of the Full-Arch prosthesis. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
The images above show a classic PFM prosthesis supported by four implants. The restoration has been successfully in place for over five years. This is an example of optimally executed work, considering the height and overall configuration of the prosthesis. Such a prosthesis will not act as a massive lever and transfer excessive load to the implants. However, it is not ideal either. Given the volume of the metal frame, veneering material will be thin. This results in frequent chips, cracks, and frequent requests for correction.
The following images show a much more complex situation. This is a temporary denture for immediate loading, made directly without the need for a dental laboratory. Note the height of this denture.

A temporary prosthesis for immediate loading made directly – the very large height and thickness of the prosthesis will inevitably cause problems with overloading of Full-Arch implants. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
Such a high and massive structure acts as a lever, and the likelihood of deformation or even fracture of the alveolar process is very high. The photo shows a relatively lightweight polymer structure. Now imagine what would happen if we replicated the same structure in zirconium dioxide. We would end up with a massive and extremely heavy structure with zero elasticity, which would inevitably destroy the bone tissue that supports the implants.
Neither option is ideal, but all other things being equal, the first option is more promising. The implants will remain stable, and the prosthesis can be redesigned. For example, a zirconium arch and multi-unit abutments with an ultra-low V-type profile from XGATE Dental, a German manufacturer specializing in multi-unit solutions, would be used to keep the screw access holes as small as possible and the prosthesis walls as thick as possible.

Comparison of prosthetic wall thickness using classic D-type multi-unit abutments (left) and MUA with a reduced V-type cone (right)
Multi-unit abutments of this type give more freedom, especially in difficult situations. For example, a deficit of space between the base of the implant and the antagonist teeth.
Of course, the example in the illustration above doesn’t apply to cases of total dentures, but similar situations may arise in practice. For example, when only one jaw requires restoration, while the other has been previously restored, or there are still healthy natural teeth or bridges present.
The following illustration shows not only exactly how this case was solved but also the general concept of working with V-type multi-unit abutments.
- Occlusion analysis. An equally important stage, this one assesses dental defects relative to the opposing jaw, pathologies, and occlusal characteristics, as well as determines whether the patient has bruxism or other jaw parafunctions. Restoration can solve many of these problems, but it presents a challenge for the dentist, especially the prosthodontist. If the patient has skeletal abnormalities or dental deformities, restoration becomes a creative task. This is especially true if only one jaw needs to be treated. In such cases, damage to the prosthesis, fractures of screws, and even abutments are common.

An example of dental arch deformation is a serious problem for a prosthodontist. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
Therefore, all identified deviations must be taken into account when planning surgery, and, if necessary, an orthopedic diagnosis must be performed to determine the feasibility of appropriate prosthetic treatment. Only then should treatment begin.
- Antagonist analysis. Let’s look at an example: the images below show a temporary restoration of the mandible supported by four implants. The right image clearly shows wear on the crowns, and even a portion of the cantilever section has broken. This is because the patient has PFM bridges in the upper chewing areas. It is much harder than PMMA plastic, and the doctor overlooked this.

Critical wear of a temporary mandible denture – the doctor did not take into account the difference in the hardness of the materials of the temporary denture and the PFM of the maxilla dentures. YouTube/ Dr. Sergey Rozhnov /sergiodontologist
It’s worth noting, however, that sometimes making dentures from materials of varying hardness is a justified solution. For example, when performing staged dentures for the maxilla and and the mandible. If one jaw already has a denture made of zirconia, then to reduce the impact load when the jaws close, the dentist may install a PFM denture or even a composite-coated framework on the other jaw. While a softer material will wear out faster, this is a good solution if osseointegration in the second jaw is not yet complete.
How to choose an implant design
First, it’s necessary to determine bone density as accurately as possible. Unfortunately, before surgery, bone type can only be determined by indirect signs. Nevertheless, the surgeon should have a general picture before the procedure.
| Bone type | Brief description | Tactile analogue | Shavings during drilling + localization |
|---|---|---|---|
| D1 | Hard and thick cortical layer, almost no spongy bone. | Oak, plywood | White shavings without blood. Usually the frontal part of the mandible. |
| D2 | Moderate cortical thickness (1.5-3 mm), dense trabecular bone | Pine, birch | White shavings with blood. Frontal maxilla or distal mandible. |
| D3 | Thin porous cortical bone (< 1.5 mm), porous trabecular bone | Chipboard | Red shavings. Distal maxilla, sometimes distal mandible. |
| D4 | Cortical layer almost absent (~0.5 mm), loose trabecular bone | Polystyrene foam, drywall | Almost no shavings; bone tissue is crushed/compacted. Distal maxilla. |
Based on bone density, the most important parameter is the thread design:
- Implants for cortical fixation: They have a low thread profile (0.3-0.4 mm average) with a rounded or rectangular thread shape. Designed for D1-D2 hard bone.
- Cancellous implants: For fixation in loose bone (D3-D4). They have a wide, aggressive thread to increase the contact area with the bone tissue.
The typical clinical picture is relatively dense bone tissue in the mandible (D1-D2) and rather loose bone with a poorly defined cortical layer in the maxilla. It’s safe to choose cortical implants for the mandible and cancellous implants for the maxilla, but not vice versa. A cortical implant in loose bone will not provide acceptable primary stability, and a cancellous implant in D1 bone will be almost impossible to place; it will become stuck or inserted with a supertorque of 70 Ncm or more.
Most patients have average bone density, and extremely hard D1 bone is not found in everyone, just like the soft D4 bone. However, D4 bone is still more common, especially in older patients.
But the point is different: In most clinical cases, we’re dealing with bone in transitional stages from D2 to D3, and identical implants with a hybrid design can be used. For example, consider the design of XGATE Dental’s X11 series implants with a conical interface. Let’s take a closer look at why this is the case.

XGATE Dental X11 dental implant section: dual threads with variable profile, reverse taper neck with micro-threads, signature Pure & Porous (P& P) surface
The reverse taper neck relieves excess pressure on the densest part of the bone (the cortex), and the micro-threads promote osseointegration. The cortex already has relatively few vessels, and without the neck’s ribbed shape, the pressure would be excessive. Instead, we have protrusions that are in close contact with the bone and depressions that fill with biological fluids, where new bone formation begins.

Implant-to-bone and bone-to-implant pressure vectors during installation of XGATE implants with reverse thread cone
The variable thread profile combines the advantages of both designs. At the tip, the threads are sharp and aggressive, facilitating insertion. As the implant is inserted, the threads widen and become rectangular. This compacts the trabecular bone and ensures good primary stability even in D4 bone or extraction sockets.

The variable thread profile of XGate implants: thin threads with a cutting edge at the beginning and gradual widening and flattening of the thread edge, this approach allows for good primary stability in most types of bone tissue.
In the next part, we’ll discuss the rules for choosing the position for implant placement, as well as selection criteria based on diameter, length, macro- and microrelief. We’ll also discuss the choice of abutments and why the concept of multi-unit abutments is being increasingly discussed in the dental community.
Disclaimer: Any medical or scientific information provided in connection with the content presented here makes no claim to completeness and the topicality, accuracy and balance of such information provided is not guaranteed. The information provided by XGATE Dental Group GmbH does not constitute medical advice or recommendation and is in no way a substitute for professional advice from a physician, dentist or other healthcare professional and must not be used as a basis for diagnosis or for selecting, starting, changing or stopping medical treatment.
Physicians, dentists and other healthcare professionals are solely responsible for the individual medical assessment of each case and for their medical decisions, selection and application of diagnostic methods, medical protocols, treatments and products.
XGATE Dental Group GmbH does not accept any liability for any inconvenience or damage resulting from the use of the content and information presented here. Products or treatments shown may not be available in all countries and different information may apply in different countries. For country-specific information please refer to our customer service or a distributor or partner of XGATE Dental Group GmbH in your region.