Contents
In the previous part, we examined which implant shape is best suited for different bone densities and the intended use of cortical and cancellous implants. In this section, we will continue to explore the rationale behind implant selection through clinical case studies. We will also touch on the physics and biological processes involved in implant placement.
Revisiting torque and stability when placing different types of implants
Let’s start with cortical implants. More precisely, with so-called supercortical implants. We already know that the stability of such implants is determined by the contact of the implant neck (collar) with the cortical layer. The implant design shown below is intended for the most common bone types, D2–D3. It necessarily includes microthreads on the implant neck to reduce pressure and trauma in the densest layer of bone.
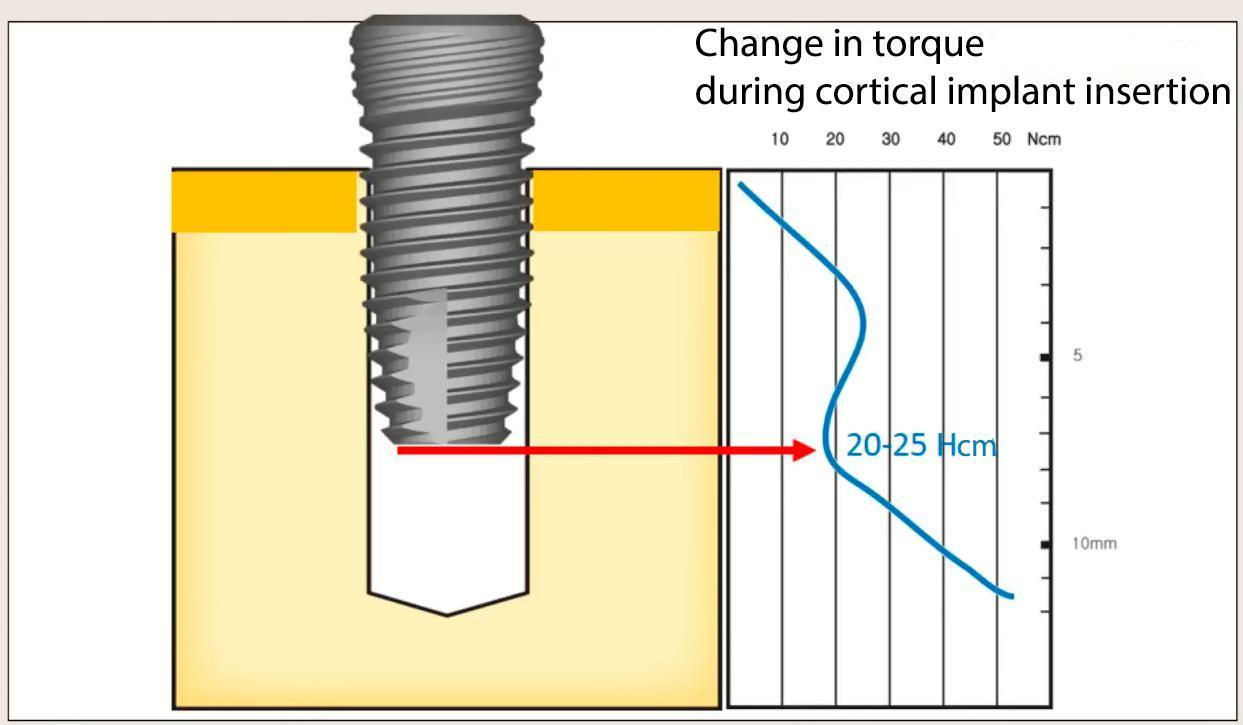
Torque versus implant insertion depth—torque reaches its maximum when the implant neck enters the cortex. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The thinner the cortex, the more tapered the implant neck should be. However, the ability to retain an implant in the cortex is limited. When there is almost no cortex (bone density between D3 and D4), the implant can only be retained in cancellous bone. In this case, cancellous implants with a wide, aggressive thread profile are required, but we will discuss these later.
For D1 bone, where the cortical bone is almost continuous, a different design is used with shallow threads and a smooth, tapered implant body. However, again, much depends on the clinical case and the implant placement method.
Why are different cortical implant designs needed?
The table below shows the design variations of cortical implants only.
| For D1 bone | For D2-D3 bone | For the split crest technique |
|---|---|---|
 |
 |
 |
| A reverse taper neck without micro-threads is the simplest and most cost-effective option. | Expanding neck with microthreads (supercortical implant). | A distinct conical shape (wedge-shaped) ideal for insertion into the split ridge. |
As we mentioned in the first part of this article, there are no perfect implants, but it is possible to choose the perfect one for a specific clinical case. Therefore, even when working with approximately the same bone type, it is possible to choose implants with different designs and purposes.
Why is a reverse taper implant neck better for D1 bone?
The picture below shows an ideal D1 bone scenario, for which a simple-shaped implant with a reverse taper in the implant neck area would be suitable.

An example of implant placement planning for D1 bone. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
For such clinical cases, implants with a simple profile and a tapered neck are the ideal choice; see examples below.

A specialized implant for dense bone (left) and a universal implant from XGate Dental, the X3 series (right).
As seen in the illustration above, the implants are very similar in shape. The key differences are in the thread profile: a single, very shallow thread profile in the specialized implant for dense bone (left) and a double-lead thread with a variable profile in the XGate implant, plus microthreads on the implant neck.
Both options are suitable for:
- Flapless implantation into D1, D2 bone.
- Simple and affordable implantation into an “ideal” ridge.
Additionally, the narrowing of the neck (reverse taper) reduces the pressure in the densest part of the cortical bone, minimizing the risk of overload and compression necrosis.
The second advantage is that it is much easier to achieve dual platform switching on this type of implant; see the illustration below.

An example of organizing double platform switching due to the correct shape of the implant and abutment.
Another important point is that the price of implants with this design is among the most affordable. This doesn’t mean they are inferior to more expensive ones; with the right choice, the survival rate is among the highest. It is simply a mass-produced product utilizing proven technology, so each unit is inexpensive while boasting high manufacturing precision and a clean, porous surface.
Cancellous implants
These are designed for soft bone with little cortical bone. Primary stability is achieved through friction between the threads and the cancellous bone.

The principle of achieving primary stability with a cancellous implant in low-density D3-D4 bone. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Here too, there are several varieties and transitional forms. Some are interesting, some are more exotic, but most clinical cases can be resolved with standard solutions.
Here are the most interesting designs of cancellous implants:
| For D3 bone | For D4 bone |
|---|---|
 |
 |
| Hybrid (semi-cancellous) implant: Neck with expansion and micro-threads for fixation in the cortical layer, and aggressive threads for engagement with cancellous bone. | A classic cancellous implant: Features wide threads and a wide thread pitch for stable fixation in loose bone. |
Let’s briefly discuss whether it is possible to use one type of implant in different bone types. Yes, it is possible. However, as discussed in detail in Part 1, using cortical implants in loose bone will result in relatively low torque and poor primary stability. This is acceptable for a delayed loading protocol, but the time for complete osseointegration increases significantly (on average, +2 months).
Conversely, placing a cancellous implant in D1 bone will be very challenging. If the osteotomy is prepared according to the standard protocol to fit the implant diameter, the implant may become stuck. If the socket is over-widened, the implant will only be held in place by the very tips of the threads, leaving large voids between the implant body and the socket walls. Given that dense bone is already poorly vascularized, bone growth will be slow, increasing the risk of fibrous integration rather than osseointegration.
In D2 and transitional D2-D3 bone, placing a purely cancellous implant will present fewer challenges, although insertion will be physically more demanding due to torque resistance.

The problem of choosing an implant design for different bone types: on the left are cortical implants for all areas of the jaw; on the right are cancellous implants for all areas of the jaw; in the center is a universal implant for most clinical cases (XGate Dental with a V-type multi-unit). YouTube / Dr. Kamil Khabiev / Dental Guru Academy
There are two ways to solve this problem:
- Use universal or transitional implant shapes. One option is a design like XGate Dental.
- Place cancellous implants in the upper jaw, where the bone is looser, and cortical implants in the lower jaw, as shown in the illustration below. We will discuss several clinical examples of such restorations below.
Long-term results of implantation: The right choice of implant design
The following photo shows a restoration 9 years post-op, and the bone level around the implants has remained virtually unchanged. Several factors were at play here:
- Correct load distribution: The upper jaw is divided into 4 bridges and has a sufficient number of implants (10 units).
- Sufficient bone volume between the implants: A distance of at least 3 mm ensures good blood supply to the bone tissue, which is crucial for long-term stability, as confirmed by this image.
- The right choice of implant design: The implants are well integrated, and this restoration can last for many more years without significant changes.

An example of a successful restoration with minimal bone loss around the implants 9 years after implant placement. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Conversely, there are examples of poor implant selection. The image shows cortical conical implants designed for a ridge-splitting protocol. They were placed in dense bone, but due to excessive pressure at the implant neck, significant bone volume was lost even before the healing abutments were placed. Now they need to be removed, the implant site remodeled, and new implants placed.

Significant bone loss during implant placement due to a design error; implants designed for the ridge-splitting technique were placed into the bone without splitting. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Another example in the image below shows significant bone loss due to incorrect implant design. This is a mandible, and at the time of implant placement, the cortex was distinct and fairly thick. Implants with a microthreaded neck designed for cortical bone anchorage should have been used—perhaps the previously discussed reverse-taper implants. In that case, the cortical bone would not have been damaged and would have been preserved in sufficient volume.

Bone loss in the lower jaw is also due to pressure from the implant neck on the cortical layer and its inevitable resorption. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Implant placement immediately after tooth extraction: Clinical examples
Let’s look at the rules and specifics of implant placement during immediate implantation protocols. The implant shape is crucial here. For example, in the position of the central or lateral incisors, the implant bed is quite narrow. The illustration below shows a tapered-cylindrical implant with a flat apex. If the implant had a pronounced conical shape during placement, there would be a risk of slipping toward the vestibular wall. However, this implant fits neatly and tightly into the prepared bed almost immediately, achieving high-quality apical anchorage.
Recall anatomy: the walls of the socket after tooth extraction are also cortical bone. Therefore, if the tip of the implant is embedded 4–5 mm into dense bone, in most cases, this provides sufficient primary stability for immediate provisionalization.

Examples of optimal implant placement in different conditions: in the anterior region, palatal positioning relative to the extraction socket is important; in the posterior regions, contact with the lateral walls or fixation in the interradicular septum is important. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The double-lead thread and a domed apex of the XGate implant also perform well in the immediate implantation protocol, in both the anterior and posterior regions.

Two Spiral Channel & a domed apex (head/top). XGate’s implant is composed of a domed apex that provides high tolerance, and two cutting blades at the bottom that provide selfscrewing properties. This enables a simpler, quicker, and, more importantly, safer procedure.
The following picture shows implantation into the socket of a multi-rooted tooth, specifically into the interradicular septum. As seen in the right picture, taken several months later, the implantation was more than successful.

An example of immediate implantation into the interradicular septum with successful integration. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Here is another clinical case where differentiated selection of implants allowed the patient to have implants and restorations placed on the same day.
The initial clinical situation is complex, with moderate bone atrophy in the upper jaw, and the bone is of very low density: D3 in the anterior region and D4 in the posterior regions. The old restorations rested on the roots of natural teeth, which had become damaged and needed to be removed. The patient experienced discomfort and pain.
In these circumstances, a delayed protocol with a removable denture placed during the healing period is typically recommended for the upper jaw. The lower jaw is in better condition, making immediate implantation with immediate loading an option. However, the patient’s request was clear: to leave with “teeth” on the day of implantation.

The initial situation: the restoration is worn out and loose, the tooth roots are decayed, and there is inflammation. Complete extraction of the remaining teeth and a permanent restoration supported by implants is indicated. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
This would not have been possible without the concept of cortical and cancellous implants.

The concept of optimal implantation planning and segmentation of restorations: lower jaw cortical implants, upper jaw cancellous implants + anatomically correct segmentation of bridges. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The images below show the implants placed according to the above-mentioned scheme. In the upper jaw, 10 cancellous implants were placed, 8 of which are used to support the temporary prosthesis. The 2 distal implants were placed with insufficient torque and were not loaded. In the lower jaw, 8 implants were placed, 6 of which are used to support the temporary prosthesis for the same reason.

Orthopantomogram of successful placement of cancellous (upper jaw) and cortical (lower jaw) implants. YouTube / Dr. Kamil Khabiev / Dental Guru Academy

Temporary restoration of the upper and lower jaws placed on the day of implantation. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
After three months, osseointegration was successfully completed, secondary stability was sufficient for the placement of a permanent restoration, and here is the result.

Fitting a permanent restoration: There is a problem with the fit of one of the bridges—the crown is overhanging the implant. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The result isn’t perfect; as you can see from the image, there were issues with one bridge—it didn’t seat properly on the distal abutment. This isn’t a major issue. The bridge segmentation concept worked to its advantage here, too. The doctor removed the problematic bridge, trimmed one crown, and then performed a single-tooth restoration on that implant.

Final permanent restoration with corrected defects in quadrant 4. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
If the restoration had been done as a continuous full-arch splint, the entire prosthesis would have had to be removed due to a problem with one crown. But with this approach, one bridge was removed, modified, or remade, while the patient could use the other side of the jaw.
As a result, the patient is happy and can eat any food with virtually no restrictions.
Here’s what the situation looks like five years later. The prosthesis is fine, but there is still some work to do on the soft tissue, and some gum grafting is needed. But that’s a topic for another article.

A follow-up photo taken 5 years after the restoration. The aesthetics and functionality are excellent, but there are some gingival defects, and the abutment collars are visible in some places. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
To be fair, I should note that there are a few issues with the dental lab work. The bridges are well-made but not perfect. However, these are typical, functional restorations, not exhibition pieces. Furthermore, the cost of these restorations is not exorbitant.
All of the above arguments confirm that a practicing clinician should have more than one implant system or design in their arsenal. There should always be a choice for a wide variety of clinical situations.
Here’s another clinical example. The patient also expressed a desire to leave after the surgery with her teeth intact. The initial clinical picture was quite dire.

The initial clinical situation: the remaining natural teeth are practically hopeless; both jaws require extraction and prosthetics. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
In this case, we’ll only briefly present the results. The point is that the same principle was adopted here: cancellous implants for the upper jaw and cortical implants for the lower jaw.

The appearance of a temporary denture immediately after placement. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
That’s all for now. In the next section, we’ll discuss the rules for using short implants and which implants to choose to avoid sinus lift surgery. All of this will also be based on clinical examples. Stay tuned for our next publications.
Disclaimer: Any medical or scientific information provided in connection with the content presented here makes no claim to completeness and the topicality, accuracy and balance of such information provided is not guaranteed. The information provided by XGATE Dental Group GmbH does not constitute medical advice or recommendation and is in no way a substitute for professional advice from a physician, dentist or other healthcare professional and must not be used as a basis for diagnosis or for selecting, starting, changing or stopping medical treatment.
Physicians, dentists and other healthcare professionals are solely responsible for the individual medical assessment of each case and for their medical decisions, selection and application of diagnostic methods, medical protocols, treatments and products.
XGATE Dental Group GmbH does not accept any liability for any inconvenience or damage resulting from the use of the content and information presented here. Products or treatments shown may not be available in all countries and different information may apply in different countries. For country-specific information please refer to our customer service or a distributor or partner of XGATE Dental Group GmbH in your region.