Contents
Research on straight and angled MUAs (0°, 17°, 30°)
In this article, we will analyze how the load on dental prostheses is distributed across the components of the restoration. We will determine under what conditions the risk of screw breakage increases and which screw will break first: the abutment screw (securing the abutment to the implant) or the prosthetic screw (securing the prosthesis to the MUA). Our primary source for this analysis is a preprint study published on Research Square. The relevance of this problem is related to the growing popularity of All-on-4, All-on-6, and other full-arch prosthetic solutions utilizing MUAs. In such operations, distally located implants are typically placed at an average angle of 30°. To compensate for this angulation, angled multi-unit abutments are used.
Learn more about the full range of multi-unit abutments.
The relevance of this problem is related to the growing popularity of All-on-4, All-on-6, and other full-arch prosthetic solutions utilizing MUAs. In such operations, distally located implants are typically placed at an average angle of 30°. To compensate for this angulation, angled multi-unit abutments are used.
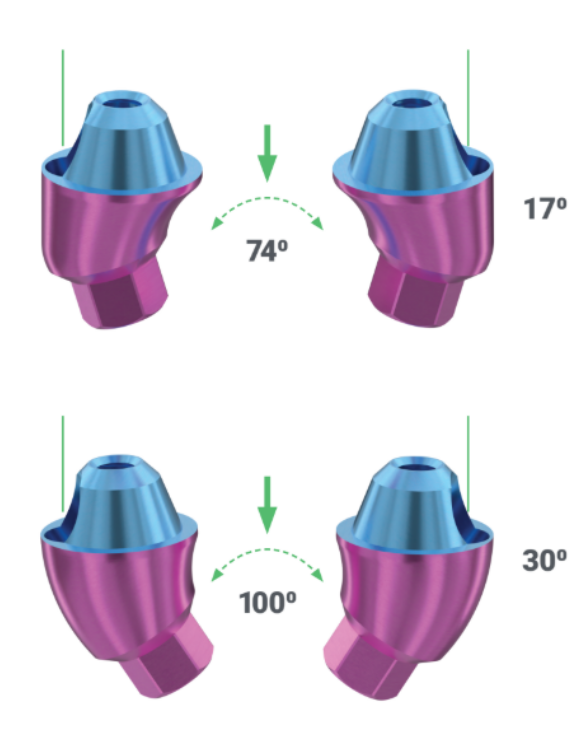
XGate 17° and 30° angled abutments are capable of compensating for implant angulations of up to 74° and 100°, respectively
However, high-quality studies on the distribution of loads on abutments, retention screws, and bone tissue around implants have been scarce. This study is particularly interesting because it paid special attention to angled abutments, which can act as a lever, transferring significantly greater loads to the implant compared to straight abutments. The purpose of this study is to determine precisely how the load is distributed and which parts are at the greatest risk. Beyond simply quantifying the increased load, horizontal loading creates significant stress concentrations in both mechanical components and the surrounding bone tissue.
How bone resorption is related to axial and lateral loads on the implant
Partial loss of bone tissue around the implant is inevitable. A loss of up to 1 mm of bone ridge height around the implant neck in the first year after surgery is considered normal, with subsequent slowing of bone loss to nearly zero. If, five years post-implantation, bone resorption around the implant does not exceed 2 mm, this is considered a successful outcome. Without sufficient bone tissue, the restoration will not achieve the estimated 15-20 year service life, which is the current goal and new standard for prosthetics.
One of the key factors in bone tissue destruction is excessive and uneven loading on the implant. When restoring a full arch, some implants are almost always placed at a significant angle relative to the dental arch. This angulation is then compensated for by angled abutments. In this position, the screws, the abutment, and the implant itself are subjected to significant overloads associated with the use of angled abutments. This contrasts with implants placed parallel to the roots of natural teeth, where more physiological axial loads prevail. For example, such a situation is typical for All-on-4 and All-on-6 protocols, as shown in the illustration below.

Straight and angled abutments in the restoration of a full arch according to the All-on-4 protocol (image from shutterstock)
For guidance on selecting the correct angulation, see our post on choosing angulated MUAs.
Let’s take a closer look at what loads increase the risk of bone tissue destruction around implants.
Why the impact on bone loss under axial loading is minimal
- Natural Direction of Load. Axial loads (i.e., directed along the axis of the implant) are considered physiologically more favorable for bone tissue. This direction of load is more natural for bone, as it imitates the load that natural teeth experience during mastication.
- Uniform Load Distribution. When the load is distributed along the axis of the implant, the force is uniformly transferred to the surrounding bone tissue. This helps maintain bone density and minimizes the risk of resorption. Conversely, in some cases, bone tissue compaction can occur around the implants, due to what is known as bone conditioning. The walls of the trabeculae thicken, and the marrow spaces may become smaller. However, this physiological phenomenon is observed only with moderate loads. If the load on the bone tissue exceeds a certain level, bone tissue resorption occurs.
- Less Risk of Micromovements. Axial loads are generally less likely to induce micromovements of the implant within the bone, which is important for osseointegration and long-term stability of the implant. Micromovements can lead to disruption of the bone-implant interface, which can cause inflammation and resorption.
Explore our guide on preliminary digital modeling for D-type MUAs.
Lateral loads pose a high risk of bone resorption around the implant
- Uneven Force Distribution. Lateral (or horizontal) loads generate forces that are unevenly distributed across the implant surface. This can result in increased loading on certain areas of the bone, which stimulates bone resorption in those areas.
- Risk of Micromovements and Instability. Lateral loads promote micromovements of the implant, especially if the load is significant or frequently repeated. This interferes with osseointegration and can lead to the formation of microfractures in the bone, which promotes resorption.
- Inflammation and Peri-implantitis. Constant lateral loads can cause microtrauma and subsequent inflammation of the tissues around the implant, which in turn can lead to peri-implantitis – an inflammatory process that is accompanied by bone resorption and almost inevitable implant loss.
- Adverse Loading on Implant Threads. Lateral forces can also adversely affect the implant threads, which over time can lead to implant loosening and loss of stability. This further increases bone resorption.
In any case, it is worth remembering the difference between a natural tooth’s root and a dental implant. A natural tooth is held in the periodontal ligament, which acts as a shock absorber and dampens sharp impacts and local load increases. The loads are thus transferred to the bone with attenuated force. In addition, a natural tooth’s support complex has high proprioceptive sensitivity. A person can detect a foreign object between their teeth if its thickness is ≥ 0.2 mm. Therefore, they can more precisely regulate chewing forces.
The implant is integrated directly into the bone tissue, and the entire load is transmitted directly to the bone. Furthermore, the reduced proprioceptive sensitivity can lead patients to exert excessive chewing forces unknowingly.
And when we add to this the design of the prosthesis, which converts axial load components into lateral ones due to the angled abutment, the risk of bone destruction due to excessive loads increases. The study we reference aims to quantify how much the lateral load increases with varying abutment angulations. This information is valuable for practicing clinicians. Perhaps in some clinical situations, it is better to perform sinus lift or guided bone regeneration (GBR) and place implants perpendicularly or with a minimal angle to the dental arch.
The research on which this article is based shows that an abutment tilt of 17° and especially 30° significantly increases stress in the bone/implant/abutment system. When horizontal forces are introduced (e.g., during lateral chewing movements), the situation deteriorates significantly. This is especially important to consider when prostheses are supported by multiple implants, in bridge structures, and in aesthetically critical areas.
Thus, for any implantologist, it is crucial not just to “place an implant,” but to understand the biomechanics of the entire structure, choosing the appropriate abutment angulation, number of implants, and prosthesis design. We will elaborate on this further.
What was studied: the purpose and objectives of the work
The main hypothesis of the study
The study, “Influence of horizontal forces on implants with different multi-unit abutment angulations: A finite element analysis,” aimed to identify how the MUA tilt angle affects stress distribution in the implant-abutment-prosthesis system under varying load directions. In particular, situations were studied where the force acts not only vertically (along the axis), but also at an angle – as occurs in real-life chewing or clenching.
The hypothesis of the study was as follows: The greater the abutment angulation, the higher the biomechanical load within the implant-abutment-prosthesis system, especially in the presence of horizontal force components. This hypothesis was tested using numerical modeling via the finite element analysis (FEA) method. The method is based on discretizing the complex geometry of an object into many small, simple elements (such as triangles or tetrahedrons) where the equations of mechanics (or other physical processes) are solved approximately. These solutions are then combined to obtain data on the behavior of the entire system. Despite being conducted on a virtual system, the results exhibit high accuracy.

The MUA implant complex models with different angulations (0°, 17°, and 30°). A, 3D model and detailed components of MUA – implant complex with different angulations. B, The section profile of implant-bone models with different implant angulations. C, The meshed models of the MUA-implant complex and bone. Research Square/ rs-4446322/v1/ Dong Lin/ Jun 2024
What clinical situations were simulated?
To enhance clinical relevance, the following situations were simulated in the study:
- Three MUA angulations: 0°, 17°, and 30°.
- Three force directions: vertical, inclined (45°), and horizontal (90°).
- A constant load of 300 Newtons (simulating physiological chewing force).
- Standard titanium implant, 4.1 mm in diameter and 10 mm in length.
- Bone tissue was modeled as a dense cortical and cancellous (spongy) structure.
Thus, each model is as close as possible to clinical reality: where axis correction is required and under natural loads.
Materials, equipment and methods used
Finite Element Analysis (FEA): why does a dentist need it?
Finite Element Analysis (FEA) is a numerical method that allows predicting the distribution of stresses and strains in a structure under the influence of external loads. In medicine and dentistry, it is increasingly used as a preliminary analysis tool, especially where conducting a clinical trial is difficult or ethically controversial.
Why is this important for a doctor? Because such studies allow clinicians to visualize what is not visible on CT and X-rays — internal overload zones, vulnerable points, potential failure points. This is especially valuable when choosing between a straight and an angled abutment, when a mistake can be costly — literally and figuratively.
What parameters were modeled?
The following parameters were taken into account in the test model:
- Abutment type (straight 0°, angled 17°, angled 30°).
- Point of force application and its direction (vertical, 45° angled, horizontal).
- Bone density.
- Material properties: titanium, zirconia, bone tissue.
- Component interfaces: screw connection between implant and abutment, cement retention between abutment and prosthesis.
All materials were assumed to be linearly elastic and isotropic, a simplification acceptable for calculation purposes.
Model design: types of implants, abutments, loads
| Parameter | Meaning |
| MUA Angulation | 0°, 17°, 30° |
| Load Type | Vertical, 45°, Horizontal |
| Load Magnitude | 300 Newtons |
| Implant | Titanium, Ø4.1 mm, length 10 mm |
| Bone | Outer cortical layer, inner cancellous |
| Connection Type | Screw abutment connection |
What the simulation showed: key findings
Effect of tilt on stress in abutments and implants
One of the most important findings of the study is a significant increase in stress in the system with increasing abutment angulation. At 0° angulation, the load distribution remained within safe limits and was concentrated in the central axis of the implant. However, even at 17° angulation, the following was observed:
- Increased stress at the implant neck.



The stress distribution of the implant of the MUA-implant complex with different abutment angulation (0°, 17° and 30°). A, The stress distribution of implants under loading condition A, B. The stress distribution of implants under loading condition B.C, The stress distribution of implants under loading condition C. Research Square/ rs-4446322/v1/ Dong Lin/ Jun 2024
- Stresses shifted closer to the cortical bone surface.
- Maximum load was concentrated in the screw connection.
When the angulation reached 30°, the situation became critical. The following arose:
- Localized overload zones at the abutment screw level.

The stress distribution of the MUA with varies abutment angulation under loading condition A, condition B and condiction C. Research Square/ rs-4446322/v1/ Dong Lin/ Jun 2024

The stress distribution of the prosthesis abutment of the MUA-implant complex models with different angulation (0°, 17° and 30°). A, The stress distribution of the prosthesis abutment under loading condition A. B, The stress distribution of the prosthesis abutment under loading condition B. C, The stress distribution of the prosthesis abutment under loading condition C. Research Square/ rs-4446322/v1/ Dong Lin/ Jun 2024
- Shifting of the load to the outer cortical bone.
- Prerequisites for marginal bone resorption.
Important: The stress levels in some cases exceeded the yield strength of titanium, which means there is a risk of screw deformation or fatigue failure of connection components.
How horizontal forces increase load
Angled or horizontally directed forces significantly amplify the effect of abutment angulation. This is especially critical when chewing in the lateral sections, where the force acts perpendicular to the implant axis. The study noted:
- Stresses under horizontal load in a 30° abutment were 2-3 times higher than with vertical loading.
- The highest concentration was found at the screw head and the internal thread of the implant.



The stress distribution of the screws (abutment screw and prosthetic screw). A, The stress distribution of screws under loading condition A. B, The stress distribution of screws under loading condition B. C, The stress distribution of screws under loading condition C. Research Square/ rs-4446322/v1/ Dong Lin/ Jun 2024
- The abutment-implant interface experienced shear and torsional forces, leading to loosening and micromotion.
Conclusion: The greater the angulation, the higher the risk of compromised connection integrity and micromovement of the structure — precursors of bone resorption and implant loss.
Clinical significance of the results
How does this affect the choice of abutment?
The simulation results highlight that the greater the angulation of the abutment, the higher the biomechanical vulnerability of the entire structure. Hence:
- Use straight MUAs (0°) whenever anatomy allows — our V-type MUAs offer up to 40° compensation with minimal overload.
- Angled MUAs (17° or 30°) are justified only when it is impossible to place the implant axially.
- When using angled abutments, it is necessary to strengthen the structure: increase the number of implants, use more robust connections, or reduce the length of cantilevers (no more than 8-10 mm).
The clinician must remember: every additional degree of angulation = additional load = additional risks.
What does this mean for prosthetic planning?
When planning the prosthetic part, especially in cases of bridge structures and full-arch prostheses on implants, it is important to:
- Avoid long cantilever sections, especially in the presence of angled abutments.
- Minimize horizontal load components by meticulously regulating occlusion and intermaxillary relationships.
- For angled abutments, consider the placement of additional implants to better distribute the load.
A prosthesis is not just a “crown on a screw.” It is a system that can either extend the life of the implant or lead to its rapid loss if the biomechanics are not taken into account.
What complications can arise if the tilt is not taken into account?
If the clinician ignores the importance of the abutment angulation and its effect on overload, the following clinical complications may occur:
- Loosening of the screw connection, potentially leading to complete unscrewing.
- Fatigue fracture of the screw or abutment.
- Marginal bone resorption, resulting in thread exposure.
- Inflammatory complications, such as mucositis and peri-implantitis.
- Ultimately — implant loss.
Important: These complications are observed more often in the distal sections of bridge structures, where the horizontal load is most pronounced.
How to apply this data in everyday practice
When to avoid angled abutments
The use of angled MUAs should be avoided if:
- There is an anatomical possibility to place the implant strictly along the axis. For example, XGate offers multi-unit abutments with an ultra-low V-type profile, which allow compensation for deviations of up to 40°, as shown in the illustration below.

The principle of using straight multi-unit V-type abutments with angulated implants
- The patient has increased occlusal load (e.g., bruxism, hypertonicity of the masticatory muscles).
- A long bridge structure is planned on 2-3 implants.
- The patient is unable to ensure proper hygiene, rendering any inflammation critical.
In doubtful situations, it is better to discuss the placement of additional implants, even if this requires a sinus lift or guided bone regeneration (GBR) procedure, than to risk overloading the angled abutment.
How to reduce horizontal forces: practical techniques
To minimize horizontal forces and their effect on angled abutments, the dentist can:
- Adjust occlusion to avoid contacts on inclined surfaces.
- Design the prosthesis with a flatter occlusal table, minimizing functional cusps/bumps on the surface.
- Prioritize rigid screw connections over cement retention — see our article on screw-retained bridges.
Accordingly, it is better if the prosthesis is:
- The prosthesis on angled abutments should be as compact and smooth as possible (avoiding large cantilevers and prominent functional cusps).
- If possible — unload distal implants by shifting the contact point anteriorly.
Comparison table of stresses at different angulations and load types
It is important for practicing physicians to have a visual table at hand in which they can quickly compare the influence of different factors on the stress level in the implant-abutment-prosthesis system.
| Abutment Angulation | Load Type | Maximum Stress Zone | Stress Value (MPa) | Clinical Risks |
| 0° | Vertical (0°) | Implant Neck | 120 | Minimum |
| 17° | Vertical (0°) | Implant-Abutment Interface | 180 | Moderate, long-term resorption possible |
| 17° | Horizontal (90°) | Screw Head and Thread | 290 | High risk of loosening and fatigue fractures |
| 30° | Vertical (0°) | Implant-Abutment Interface, Screw | 270 | Significant increase in load |
| 30° | Horizontal (90°) | Screw Connection, Adjacent Bone | 350+ | Critical overload, high probability of complications |
These data confirm that at an angulation of 30° and under lateral forces, stresses exceed safe limits, especially in the screw region and adjacent bone. This is a direct indication for the clinician to reconsider the treatment strategy.
What other studies say
A meta-analysis published in Clinical Oral Implants Research confirms that angled abutments result in increased bone resorption, especially in the first 12 months after implant loading. Other clinical reviews show:
- With angled abutments, bone resorption can reach 0.7–1.2 mm in the first year.
- The risk of screw loosening increases 2.5 times if the abutment angulation exceeds 15°.
- Designs with angled abutments often require revision or repair within the first 3 years of service.
This is consistent with the results of numerical simulations and indicates the need for caution when selecting the abutment angulation.
Conclusions
It has long been known that the load on the bone, implants, and retention screws increases when using angled abutments, but until now there were no studies with specific quantitative data. Now, both scientists and practicing dentists can use the data from this study to improve the quality of restorations supported by implants.
What to consider when choosing an abutment
- An angled abutment is not a panacea. The greater the angulation, the higher the stress and risk of complications. It is always crucial to consider how to mitigate the negative consequences and risks if the use of an angled abutment is unavoidable.
- Straight abutments are the gold standard if anatomy allows. Straight abutments come in different varieties, such as the previously mentioned V-type multi-unit abutments, which allow compensation of a significant angle of deviation without significantly increasing local overloads on all components of the restoration.

V-type abutments with standard sleeves: angulation compensation up to 40° possible
- Angled abutments should be used consciously, only when axial (vertical) placement is impossible. There are clinical cases where even 45° abutments are justified, and if all conditions are met, such restorations can be quite successful.
- Always take into account the direction and magnitude of masticatory forces, especially with lateral movements.
- Don’t hesitate to place additional implants — it may be more cost-effective than treating complications.
How to reduce risks and extend the service life of a restoration
- Utilize digital planning and preliminary modeling.
- For angled abutments — minimize the length of cantilevers.
- Customize occlusion to reduce lateral forces.
- Prioritize rigid screw connections over cement retention.
- Always conduct regular maintenance of the restorations.
Frequently Asked Questions (FAQ)
Clinical guidance on angled abutment selection, load management, and alternatives.
When is it safe to use an angled abutment?
It is considered safe when axial implant placement is impossible, but it is possible to ensure adequate load distribution (for example, via an additional implant) and minimize horizontal forces.
Why are horizontal forces so important?
Horizontal forces create torsional and shear stress at the abutment–implant interface and are common causes of loosening, bone resorption, and screw failure.
Is it possible to compensate for abutment angulation with the design of the prosthesis?
Partially. A well-designed prosthesis can redistribute the load, reduce leverage, and shift the pressure point. But it does not completely eliminate the risks associated with an angled abutment.
What angulation is considered critical?
In practice, anything above 15° requires careful assessment. Angulations of 30° and above are considered high risk, especially in bridges and distal abutments.
Is there an alternative to angled multi-unit abutments?
Yes, alternatives could include custom titanium or zirconia abutments, or the use of digital planning followed by implant placement at the desired angle using surgical templates.
Disclaimer: Any medical or scientific information provided in connection with the content presented here makes no claim to completeness and the topicality, accuracy and balance of such information provided is not guaranteed. The information provided by XGATE Dental Group GmbH does not constitute medical advice or recommendation and is in no way a substitute for professional advice from a physician, dentist or other healthcare professional and must not be used as a basis for diagnosis or for selecting, starting, changing or stopping medical treatment.
Physicians, dentists and other healthcare professionals are solely responsible for the individual medical assessment of each case and for their medical decisions, selection and application of diagnostic methods, medical protocols, treatments and products.
XGATE Dental Group GmbH does not accept any liability for any inconvenience or damage resulting from the use of the content and information presented here. Products or treatments shown may not be available in all countries and different information may apply in different countries. For country-specific information please refer to our customer service or a distributor or partner of XGATE Dental Group GmbH in your region.