Contents
There are numerous clinical cases where the placement of 10 mm or even 8 mm implants is impossible. Every practicing dentist encounters this regularly. There are two primary options: bone grafting or ultra-short implants. In this article, we will discuss which implants are considered short and what conditions must be met to ensure their stability and sufficient mechanical strength to withstand prosthetic loading. It should be noted right away that, despite all the successful cases of using short implants, if it is possible to use standard 8-10 mm implants, then those should be used. Only in cases where the choice is between risky bone augmentation surgery and the installation of short implants does it make sense to use 5-6 mm short implants.
Which implants can be considered short?
In the 1990s and early 2000s, all implants shorter than 10 mm were considered short. However, the paradigm has shifted. According to the 2018 ITI Consensus Conference, implants of 6 mm or less are now classified as short.
The fact that it is possible to work with implants of this length is confirmed by a 2010 study:
Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis — Eduardo Anitua et al. (2010)
This study, conducted on photoelastic models, found that the main load is distributed across the first 5–6 threads of the implant, corresponding to a length of approximately 5–6 mm.
Visualization of load distribution on implants using photoelastic models. YouTube/ Implantarium/ Rauf Aliyev
However, there is one important nuance: if at the time of implant placement it is completely immersed in bone tissue, say by 6 mm, then after 8-12 months there is a loss of marginal bone around the implant, and only 4 mm remain immersed in the bone. Therefore, even with bone deficiency, a length of 8 mm is considered the “gold standard.” Even with a loss of 2 mm of contact with the bone, 6 mm still remains, and the implant remains stable.
In reality, short implants have existed for quite some time. The company founded by Dr. Brånemark began producing 5 mm implants shortly after the introduction of root-form implants. Today, implants of 6, 5, and even 4 mm in length are available. It is worth discussing them in more detail.
When short implants are needed – 6 mm long or less
It is difficult to find absolute indications for the placement of short implants. While recommendations in the literature vary, there are three main clinical situations where short implants are a viable choice:
- Significant vertical bone loss or other defects that preclude the placement of standard-length implants. This frequently occurs in the posterior mandible. This is perhaps the most common indication for short implants. The alternative is vertical bone augmentation, a complex surgical procedure with a high risk of complications.
- Chronic sinusitis, allergic sinusitis, and similar conditions. Sinus lift surgery is often contraindicated for these patients, making short implants the only acceptable option. While these patients represent a small percentage of cases, the situation warrants consideration.
- Patient preference. Specifically, a conscious refusal of bone grafting surgery. Many patients choose short implants after being fully informed of the risks and complications associated with bone grafting. Even with a favorable outcome, not every patient is willing to wait 8 to 12 months for a definitive prosthesis. Short implants allow the patient to avoid grafting and receive a permanent restoration in just 4 to 6 months.
We are by no means advocating the abandonment of osteoplasty or sinus lifts; however, clinical data indicates significant complication rates:
- Classic sinus lift: 10% complications (Schwartz-Arad et al., 2004)
- Vertical augmentation using a rigid titanium mesh/membrane: 40% complications (Merli M et al., 2007)
- Inferior alveolar nerve lateralization: 21% irreversible complications (Ferrigno et al., 2005)
- Distraction osteogenesis: 75% complications (Enislidis et al., 2005)
Therefore, if it is possible to place implants without bone grafting, it is an opportunity worth taking.
How short implants can solve the problem if the complications have already occurred
As an example, we will look at a case by Dr. Marco Esposito, published in the following article:
The issue arose after a failed attempt to increase alveolar ridge height. The situation was ultimately resolved using short implants. Initially, the technique used was augmentation with xenogeneic bone blocks.

Surgery to increase the height of the alveolar ridge using a xenogeneic bone block. YouTube/ Implantarium/ Rauf Aliyev
While this technique can yield good results, in this specific case, the block was completely rejected and lost, along with the implants. Consequently, the defect became even more pronounced than it was prior to surgery.

Consequences of unsuccessful bone augmentation (bone block rejection). YouTube/ Implantarium/ Rauf Aliyev
Without going into the specifics of why the complication arose, Dr. Esposito’s team was left with a patient who had agreed to a risky surgery that failed, requiring a solution. As a temporary solution, they proposed placing short implants to rehabilitate the patient.

Placement of two short implants in the remaining bone after rejection of the bone block. YouTube/ Implantarium/ Rauf Aliyev
After the osseointegration period, Dr. Esposito’s team found that the implants were supporting the load perfectly, and the restoration was fully functional. This raises the question: why undergo risky surgery if short implants could have been placed initially?
It remains to be seen whether the use of short implants is justified and how reliable they are in the long term. However, the conclusions from Dr. Esposito’s article are clear:
Short-term data (1 year after loading) indicate that 6 mm-long implants with a conventional diameter of 4 mm achieved similar if not better results than longer implants placed in augmented bone. Short implants might be a preferable choice to bone augmentation, especially in posterior mandibles since the treatment is faster, cheaper and associated with less morbidity.”
However, a single publication is not proof that such implants work in every scenario. The purpose of this article is to examine the advantages and risks of using short implants in complex clinical cases.
What do publicly available publications say?
In the early stages of research, publications were conflicting. Some specialists reported good results, while others discouraged the use of short implants due to high complication rates and low stability.
Summarizing the findings, they showed a significant difference in survival rates: 75–80% for short implants versus 92–96% for long ones. When comparing failure rates, short implants showed a failure rate of over 60% in some early contexts.
On the other hand, there are other publications.
They noted no significant difference in survival rates over observation periods of 5 to 15 years.
But in 2006, all the controversy was resolved. That year, two remarkable French researchers, Franck Renouard and David Nisand, published the results of their study.
“Impact of implant length and diameter on survival rates”
They conducted a meta-analysis, dividing publications into those published before and after the year 2000. From the 1980s to the late 1990s, implants typically had a machined (smooth) surface. It was not until the late 1990s that rough-surface implants became widespread, and by the early 2000s, manufacturers began producing surfaces with micro-texture
Renouard and Nisand identified a clear pattern: almost all studies reporting high complication rates were performed on machined implants. Studies showing comparable survival rates between long and short implants were conducted using implants with rough surfaces.
There are other interesting findings by Dr. Renouard and Nisand:
“When surgical preparation is related to bone density, textured-surfaced implants are employed, operators’ surgical skills are developed, and indications for implant treatment duly considered, the survival rates for short and for wide-diameter implants has been found to be comparable with those obtained with longer implants and those of a standard diameter. The use of a short or wide implant may be considered in sites thought unfavourable for implant success, such as those associated with bone resorption or previous injury and trauma. While in these situations implant failure rates may be increased, outcomes should be compared with those associated with advanced surgical procedure such as bone grafting, sinus lifting, and the transposition of the alveolar nerve.”
The key takeaway for practicing surgeons is the essential importance of surgical skill. This means that short implants are not for beginners. This makes sense, as in standard cases, it’s better to use normal-length implants of 8-10 mm or more, while short implants are reserved for complex cases, where the surgeon’s skill is essential.
Experience also confirms that implant success depends on bone density. If a patient has D4 bone, the likelihood of a short implant integrating properly is unfortunately low.
There is even a study on this topic, which indicated that in soft bone, the lack of stability can be compensated for by the length of the implant.
Here is a table from this 2017 publication.
Why not all design options are suitable for short implants
Let’s start with a clinical case described by Israeli colleagues in the following article:
“Short dental implants in reduced alveolar bone height”
A large 6 mm diameter, 6 mm long implant with a standard thread profile was used. A standard profile means threads are sharper at the apex and become smoother toward the neck.
The available bone height was 7 mm to the floor of the maxillary sinus (see the illustration below).

Description of the situation: bone conditions, implant design, condition with a healing cap. YouTube/ Implantarium/ Rauf Aliyev
Many specialists note that 7 mm of bone in the maxillary sinus is a significant amount, and an implant 8 or even 10 mm long could have been used. There are numerous observations that extending the implant apex into the maxillary sinus by 2-3 mm does not lead to any complications, and over time, everything integrates and is covered with bone tissue even without the use of additional bone grafting.
However, in this case, an experiment was conducted to test a short implant under these conditions.
The implant was placed subcrestally, 1 mm below the marginal bone level. The implant apex was positioned almost at the maxillary sinus floor, as seen in the upper left slide.
Everything seemed fine: The implant was stable. However, a 12-month follow-up showed slight bone resorption, and the implant neck was exposed by about 1 mm.
Considering that the implant was initially recessed by 1 mm, the total loss is 2 mm. If the implant hadn’t been placed subcrestally, no more than 4 mm would have remained in contact with the bone, and now it’s 5 mm, which is still low, but not critically so.
Now imagine an even more complex situation where a 4 mm long implant would need to be installed. With just 1 mm of bone loss, only 3 mm of contact would remain. This is critically low, especially in the chewing area.
But there is a solution here too, namely a different implant design: Tissue Level implants. Short implants with a Tissue Level design perform exceptionally well in challenging conditions. Minimal bone loss is always observed around these implants and their “big brothers”, and often the marginal bone level is completely preserved.
Good bone health is due to the soft tissue connection that forms around the implant neck. In other cases, even double platform switching only partially reduces bone resorption.
However, Tissue Level implants require more surgical skill. If your surgeon has only placed Bone Level implants, don’t start with short implants; it’s best to seek help from a specialist who has experience with this type of implant.
Why should restorations on short implants be splinted?
Prosthetics on short implants should consist of bridges or splinted structures. Single restorations on short implants pose a significant risk and should be avoided.
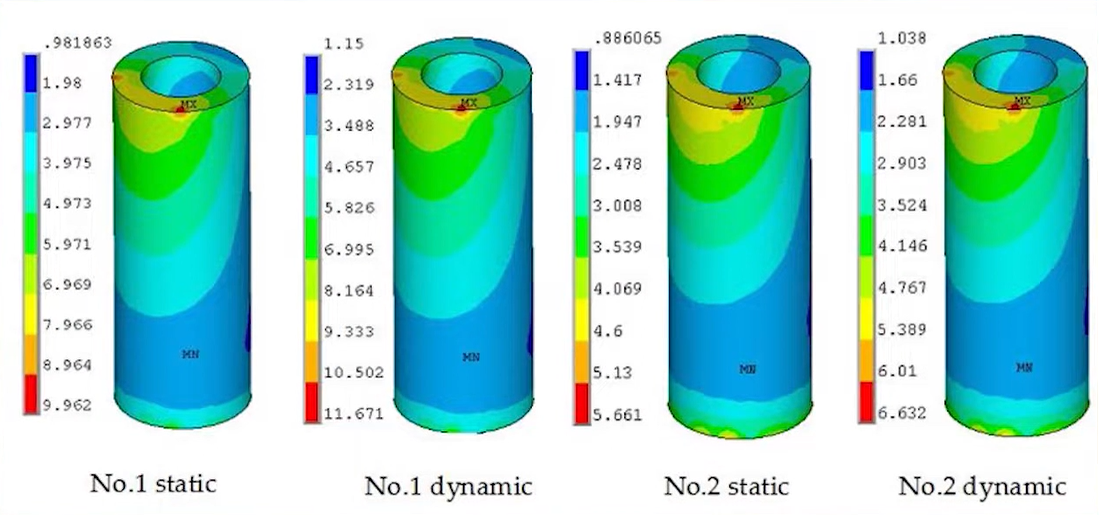
There is an interesting study on load distribution in prostheses with cantilevers:
“Additional Supplementary Support of A Short Implant for the Distal Cantilever Partial Prosthesis”
Although this study is not directly related to the comparison of single and splinted structures on short implants, it does give an idea of the loads on bone tissue.
This in vitro study involved constructing a test rig containing a simulated prosthesis with different cantilever lengths and implant positions. Loads were applied to the prosthesis, and the transfer of these loads to the implants was measured.
In the context of our article, it’s interesting to note that if a short implant is placed in the posterior region (eliminating the cantilever), the stress distribution improves dramatically. Even with a short implant in softer bone, stress is distributed more evenly, improving the long-term prognosis.
Another interesting study, though not new (dating back to 2002), noted that non-splinted restorations (when several single restorations are placed side by side) experience higher mechanical complication rates, including screw loosening, screw fracture, implant wall fracture, and abutment fracture.
“Effect of splinting and interproximal contact tightness on load transfer by implant restorations”
Here are the final conclusions, which remain valid to this day:
- Splinting effectively reduces peak stresses on the middle implant of a three-unit bridge. Non-splinted restorations concentrate stress around each implant.
- Load distribution across splinted restorations was least significant when loads were applied to the posteriormost implant. Axial loads in splinted and non-splinted restorations were similar.
- Distribution across splinted restorations was observed when loads were applied to the anteriormost implant, which was positioned slightly off-axis. This result suggests that splinting may be effective with implants positioned slightly off-axis.
- As interproximal contact density increased, the passivity of fit decreased. Increasing interproximal contact density in non-splinted restorations resulted in decreased passivity of fit.
What are the conclusions? The results of the ITI 2018 Consensus Conference
Survival rates of short dental implants (≤6 mm) compared with implants longer than 6 mm in the posterior region.
Amsterdam 2018
Final provisions of the consensus conference:
Short implants (≤6 mm) demonstrate similar survival rates compared to longer implants (>6 mm) after periods of function of 1-5 mm. The median survival was 96% (range 86.7-100%) for short implants and 98% (range 95-100%) for longer implants. A meta-analysis showed that the hazard ratio for failure with short implants is 1.29 (95% CI: 0.67, 2.50, P = 0.45). This statement is based on a meta-analysis of 10 RCTs including 775 patients (392 patients with short, 383 with longer implants) and 1290 implants (637 short, 653 longer implants).
Functional time may reduce the survival of short implants to a greater extent than that of longer ones. This assertion is based on one RCT with a 5-year follow-up, including 45 patients and 60 implants (30 short, 30 long). This is further supported by a recently published RCT with a 5-year follow-up of patients, which could not be included because it was published after the cutoff date for inclusion in the systematic review.
Short and longer implants show similar rates of radiographic changes in interdental space. After 1-5 years, radiographic changes in interdental space for short implants ranged from +0.06 to -1.22 mm, while the corresponding values for longer implants ranged from +0.22 to -1.54 mm. This statement is based on 10 RCTs including 775 patients (392 with short, 383 with longer implants) and 1290 implants (637 short, 653 longer implants). The rate of surgical and postoperative complications is higher in the longer implant group (mean: 32.8%; range: 0-90%) compared to the short implant group (mean: 6.8%; range: 0-26%)(1). In the group with longer implants, most complications were related to bone grafting procedures (2).
The longevity of prosthesis for both short and longer implants after 1-5 years is also high. The average prosthesis survival rate was 98.6% (range: 90-100%) for short implants. This statement is based on nine randomized controlled trials involving 625 patients (317 with short implants and 308 with longer implants).
Clinical recommendations:
Short implants are a suitable option in situations with moderate bone height, where it is important to avoid potential complications associated with augmentation procedures or to reduce treatment time. They may also be preferable when the risk of damage to adjacent structures can be significantly reduced.
Adjacent structures include: maxillary sinuses, blood vessels and nerves, teeth and existing implants.
When to choose short implants?
The choice of implant length depends on local anatomical features and the patient’s condition. If there is sufficient bone height, implants with a length of 8-10 mm are preferable, provided they can be placed without increasing the surgical risk.
Is it possible to load short implants immediately?
Loading times for short implants reported in the literature ranged from 6 weeks to 6 months. Currently, there are no evidence-based recommendations for immediate loading.
Does implant diameter affect the survival rate of short implants?
Based on the results of the studies included in this review, short implants with a diameter of 4 mm or greater should be used.
Should adjacent short implants be splinted?
Based on the results of the studies included in this review, a clinical recommendation is made to use splinting for the restoration of adjacent short implants.
What are the occlusal features of restoration on short implants?
Although the review literature does not provide specific recommendations regarding occlusion, the high risk of occlusal overload with short implants should be considered. Particular caution should be exercised when prescribing short implants to patients with missing single molars and/or parafunctional habits. Changes in occlusion should be assessed and adjusted, if necessary, during regular visits.
To sum up all of the above:
- Short implants are an excellent option, but only in skilled hands. In these cases, there is no room for error.
- Do not choose short implants if an 8 mm or 10 mm implant can be placed.
- Clinical performance of short implants should only be compared against long implants placed in regenerated bone (GBR), where short implants often demonstrate superior results.
- If possible, Tissue Level designs are preferable for short implants.
- Maximize the contact area for stable restorations. A short implant should have the widest possible diameter. An implant 6 mm in diameter and 6 mm in length has a bone contact area comparable to a 4 mm x 10 mm implant.
- An aggressive thread profile provides better primary stability for short implants.
We hope this article was interesting. Stay tuned for our next publication.
Disclaimer: Any medical or scientific information provided in connection with the content presented here makes no claim to completeness and the topicality, accuracy and balance of such information provided is not guaranteed. The information provided by XGATE Dental Group GmbH does not constitute medical advice or recommendation and is in no way a substitute for professional advice from a physician, dentist or other healthcare professional and must not be used as a basis for diagnosis or for selecting, starting, changing or stopping medical treatment.
Physicians, dentists and other healthcare professionals are solely responsible for the individual medical assessment of each case and for their medical decisions, selection and application of diagnostic methods, medical protocols, treatments and products.
XGATE Dental Group GmbH does not accept any liability for any inconvenience or damage resulting from the use of the content and information presented here. Products or treatments shown may not be available in all countries and different information may apply in different countries. For country-specific information please refer to our customer service or a distributor or partner of XGATE Dental Group GmbH in your region.